NNU Covid Survey #8: Year Three: Acute and Long Covid, A Double Public Health and Occupational Health Crisis
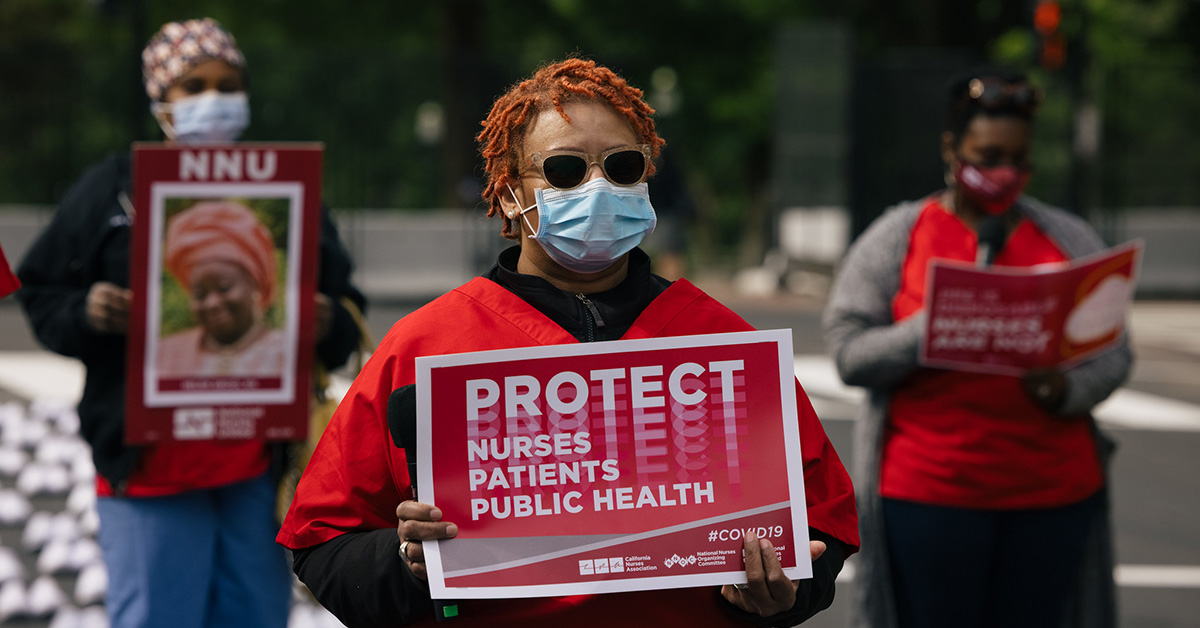
National Nurses United’s (NNU) new nationwide survey of more than 2,800 registered nurses reveals continued significant issues related to staffing, workplace violence, Covid precautions, and other issues. This survey is the eighth national survey of nurses during the pandemic by NNU.
Responses were gathered from 2,825 nurses, from both NNU union nurses and nonunion nurses in 46 states plus Washington, D.C. The results cover the period September 22 through November 28, 2022.
Covid-19: Testing and Screening
- Only 33.5 percent of nurses report that all nurses are informed of exposures in a timely fashion. 31.7 percent of nurses report that nurses are informed of exposures but not in a timely fashion. Nearly 20 percent (18.6 percent) of nurses report that nurses are not informed of exposures at all. Timely notification of an exposure to Covid-19 is essential for preventing onward transmission.
- While 71.8 percent of nurses report that patients are always screened for Covid signs and symptoms, only 37.2 percent of nurses report that visitors are always screened for Covid signs and symptoms. Even fewer nurses report that patients (49.6 percent) and visitors (7.1 percent) are always tested for Covid, despite the fact that a majority of transmission occurs before symptoms develop.
Covid-19: Personal Protective Equipment (PPE)
- Only 67.0 percent of nurses report having access to a sufficient supply of N95 or other kinds of respirators on their unit. 20.7 percent of nurses report they have access to N95 respirators on their unit but supply is not always sufficient. Ready access to PPE, including N95 respirators, is a necessary element in keeping nurses and other health care workers safe from Covid exposure.
- Only 66.3 percent of nurses report wearing a respirator for every encounter with a Covid-positive patient. It is scientifically clear that Covid-19 is transmitted through respiratory aerosols created when people infected with the virus breath, speak, cough, sneeze, etc. and that respiratory protection is a necessary element in keeping RNs and other health care workers safe from Covid-19.
- 42.8 percent of hospital nurses report having to reuse single-use PPE. While this is a decline from the April 2022 survey, which found that 62 percent of hospital nurses reported reusing single-use PPE, reusing single-use PPE is an unsafe practice that should never occur.
Long Covid
- 69.8 percent of nurses report having been diagnosed with Covid-19.
- Of those who reported having had Covid, 68.4 percent had Covid once, 22.0 percent twice, 4.9 percent three times, 1.0 percent four times, and 0.14 percent five or more times.
- After recovery from Covid-19, nurses experienced the following symptoms: tiredness or fatigue (80.7 percent), memory or concentration difficulties (52.5 percent), joint or muscle pain (51.5 percent), headaches or migraines (48.8 percent), difficulty breathing or shortness of breath (35.9 percent), symptoms that get worse after physical or mental activities (32.8 percent), heart palpitations (27.8 percent), chest pain (16.6 percent). Long Covid occurs when symptoms persist for weeks to months or new symptoms appear following a Covid infection.
- For nurses experiencing long Covid, these symptoms have lasted: 0-3 months for 31.4 percent of nurses, 4-6 months for 16.2 percent of nurses, 7-9 months for 8.1 percent of nurses, 10-12 months for 7.2 percent of nurses, and more than 12 months for 17.9 percent of nurses.
- A majority of nurses (59.9 percent) took time off work to recover from post-Covid or long Covid symptoms. 39.6 percent took less than one month off work, 5.3 percent took 1-2 months, 2.6 percent took 3-4 months, 0.45 percent took 5-6 months, and 0.98 percent took more than 6 months. About two percent (2.4 percent) are not yet back at work.
- A majority of nurses experiencing long Covid have not sought treatment for long Covid (78.2 percent). Of those who have sought treatment, only 51.2 percent have received it. The most common barrier to long Covid treatment reported was not being believed about my symptoms.
- For 37.5 percent of nurses who had Covid, their long Covid symptoms have affected their ability to work. And for 55.7 percent of nurses, their long Covid symptoms have impacted their daily activities outside of work.
- Most nurses experiencing long Covid have not made a reasonable workplace accommodation request (78.2 percent). Only 6.7 percent of nurses have made a reasonable accommodation request where it was granted. For 5.1 percent of nurses, they made a request but it was denied.
Staffing
- 56.8 percent of hospital nurses report that staffing has gotten slightly or much worse recently.
- 48.5 percent of hospital nurses report an increase in the use of travelers in the past month.
- 21.7 percent of hospital nurses report floating to/being reassigned to a clinical care area where they were expected to care for patients that required new skills or competencies. Only 16.2 percent of hospital nurses reported receiving all the clinical and educational support that they needed to practice safely and competently. Most nurses received either no education or preparation (43.7 percent) or “just in time” or “emergency” competency education (32.1 percent). These results are nearly unchanged from the April 2022 survey, indicating that hospitals continue to rely on unsafe measures to staff units.
- 10.0 percent of hospital nurses report that their facility has introduced new models of nursing, e.g., team nursing, or other “crisis staffing standards” in the past month.
- Nearly half (49.2 percent) of hospital nurses report that their facility is using excessive overtime to staff units.
Workplace Violence
- 40.5 percent of hospital nurses report a small or significant increase in workplace violence incidents recently. This is a similar level as the April 2022 survey.
Impacts of the Pandemic
Covid-19 continues to have a deep impact on the mental health of nurses, who continue to face moral distress and moral injury at work.
- 62.3 percent of nurses report they are afraid they will catch Covid-19.
- 72.1 percent of nurses report they are afraid they will infect a family member with Covid-19.
- 50.7 percent of nurses report having more difficulty sleeping than they did before the pandemic.
- 72.0 percent of nurses report feeling stressed more often than they did before the pandemic.
- 68.6 percent of nurses report feeling anxious more often than they did before the pandemic.
- 57.6 percent of nurses report feeling sad or depressed more often than they did before the pandemic.
- 47.1 percent of nurses report feeling traumatized by their experiences caring for patients during the pandemic.
- 21.9 percent of nurses report having sought treatment for a mental health condition related to caring for patients during the pandemic.
- 35.0 percent of nurses report that they are seeking or have gotten a different job.
- 55.5 percent of nurses have thought about leaving nursing.
- 75.9 percent of nurses know coworker(s) who have left nursing.
Previous surveys
In 2020, NNU’s four surveys covered hospitals’ lack of preparedness for Covid-19 (March); government and employers’ disregard for nurse and patient safety (May); the devastating impact of reopening too soon (July); and hospitals’ and health care employers’ lack of preparation for the fall/winter surge, despite more knowledge about the dangers of the virus and effective measures to prevent spread (November). In 2021, NNU’s March 2021 survey highlighted the continuing disregard of hospitals and health care employers for the safety of nurses and health care workers. The September 2021 survey revealed that employers must do more to be fully compliant with the Occupational Safety and Health Administration emergency temporary standard to protect nurses and other health care workers. The April 2022 survey revealed significant increases in unsafe staffing, workplace violence, and moral distress and showed that hospitals were still not adequately prepared for a Covid-19 surge.
December 13, 2022