Quad-demic: RSV, Influenza, Covid-19, and Crisis Standards of Care

This page was last updated on January 9, 2023
Quad-demic live conversation
Watch our conversation with NNU experts to learn what nurses and other health care workers need to know about the quad-demic we are now facing — and what is needed to protect ourselves, patients, and public health.
What nurses need to know
Currently, rates of influenza and respiratory syncytial virus (RSV) are climbing rapidly across the United States. Pediatric hospitals are full. Hospitalizations for flu are the highest for this time of year in over a decade. This is happening while the Covid-19 pandemic continues. The hospital industry’s normalizing of crisis standards of care sets the stage for the respiratory viral surges to become another crisis.
Respiratory Syncytial Virus (RSV)
RSV is a respiratory virus that infects the lungs and respiratory tract. In healthy people, symptoms are usually mild and self-limiting. Asymptomatic infections appear to be common and some individuals, including young children, can shed virus for long periods of time. In children and other vulnerable individuals, including many adults, RSV infection can cause serious illness or death.
Influenza
Influenza is a respiratory virus that infects the nose, throat, and lungs. It can cause mild to severe illness and can lead to death. Asymptomatic infections and presymptomatic transmission are common. Serious complications can happen at any age, but there are some groups at higher risk (adults over age 65 years, children younger than five years, people who are pregnant, and people with certain chronic health conditions).
Covid-19/SARS-CoV-2
Covid-19 is the disease caused by the coronavirus, SARS-CoV-2, which can infect the respiratory tract. It can cause mild to severe illness and can lead to death. Asymptomatic infections and presymptomatic transmission are common. Serious complications can happen at any age, but there are some groups at higher risk (adults over age 65 years, people who are immunocompromised, and people with certain chronic medical conditions). Anyone infected with SARS-CoV-2 is at risk of long-term health impacts (“long Covid”), which can impact every major organ system, even if their initial infection was mild or asymptomatic. SARS-CoV-2 infections can also lead to immune dysregulation for weeks to months following infection.
This is really a Quad-demic…
In addition to the three circulating respiratory viruses, a fourth factor is at play in the current crises—hospital disaster capitalism and the health care industry’s embrace of crisis standards of care. The hospital industry has implemented changes motivated by increasing profit and excess revenues and this has set the stage for the current surge in RSV, influenza, and Covid-19 patients needing care and hospitalization to be a crisis.
The hospital industry has long implemented programs to increase profits and excess revenues without regard for patient care—such as by intentionally short staffing units, closing units and facilities that aren’t “profitable” enough, and failing to prepare for infectious diseases like seasonal influenza surges and Covid-19. Additionally, for several decades, the hospital industry has desired to replace registered nurses (RNs) entirely. The hospital industry’s aim has been to deskill the nursing process by inappropriately pushing care to the lowest-cost and least-regulated setting, including retail clinics, outpatient surgery centers, and the patient’s home. The attack on nursing practice and patient advocacy includes displacing RNs and RN professional judgment with health information technology, automation, remote monitoring tools and, ultimately, abandoning the patient by leaving complex clinical care to be provided in the home by the family or even by the patient alone.
During the Covid-19 pandemic, regulatory flexibility afforded the hospital industry a rationale and opportunity to adopt—and normalize—crisis standards of care, even when not in a surge—from locking up and rationing personal protective equipment (PPE) to adopting harmful staffing models like team nursing. Hospital industry mistreatment and neglect of RNs and other health care workers has also led to many health care workers to leave their respective facilities in order to protect their health, wellbeing, and licenses, which has created a staffing crisis in health care.
The hospital industry’s decades-long campaign to increase profits and revenues without regard for patient care has resulted in a decreased number of inpatient beds, especially pediatric beds, and a nation-wide staffing crisis. The result is the current quad-demic surge.
How are RSV, influenza, and Covid-19 transmitted?
All three circulating respiratory viral illnesses (RSV, influenza, and Covid-19) can be transmitted via contact and airborne/aerosol transmission.
| Contact Transmission | Airborne/aerosol Transmission |
|---|---|
RSV, influenza, and Covid-19 infection can occur via inoculation through the eye or other mucous membranes from environmental contamination on objects.
| RSV, influenza, and Covid-19 infection can also occur by breathing in infectious airborne particles (or aerosols).
|
Immune responses to RSV, Influenza and Covid-19
Being infected with RSV, influenza, or Covid-19 does not guarantee protection from future infection.
- RSV infection confers only partial immunity and people remain susceptible to repeat RSV infections over the lifespan. There is currently no vaccine for RSV.
- Immune responses to influenza infection are relatively broad and long-lived, but influenza viruses can escape from immune responses due to their high mutation rates. There are multiple vaccines available for seasonal influenza and the level of protection provided against infection depends on how well the vaccine is formulated to match circulating strains. Typically, seasonal influenza vaccines are 40-60% effective against infection. Seasonal influenza vaccines also provide protection against serious outcomes, such as ICU admission or death from influenza and major cardiovascular events.8,9
- SARS-CoV-2/Covid-19 infection confers short-lived immune protection. New variants of SARS-CoV-2 continue to emerge and spread, often with increased immune escape and/or transmissibility. Reinfections are increasingly common. There are multiple vaccines available for SARS-CoV-2/Covid-19 with protection against infection, hospitalization, and death initially strong but then quickly fading over time. Additional boosters have been developed, including most recently the bivalent booster updated to match the Omicron BA.4/5 variants. Boosters have helped restore vaccine effectiveness, but uptake of the bivalent (updated) booster has been low.10
Why is the surge in flu and RSV hospitalizations so bad this year?
Public health measures adopted to slow the spread of Covid-19 also helped reduce the spread of other respiratory viruses in 2020. However, those public health measures are no longer in place, so it is not surprising to see a surge in respiratory viral illness transmission. It is likely that immune dysfunction caused by Covid, reinfections, and long Covid is also playing a role in causing the significant impact of RSV on young children and infants and influenza on the general population. At least 75% of children and adolescents have had Covid at least once. Additionally, the closure of pediatric hospitals and units has restricted the number of beds available nationally, contributing to the surge in pediatric hospitalizations.
Read more in NNU’s statement here.
What protections do nurses and caregivers need to care for a patient with RSV, influenza, and/or Covid-19?
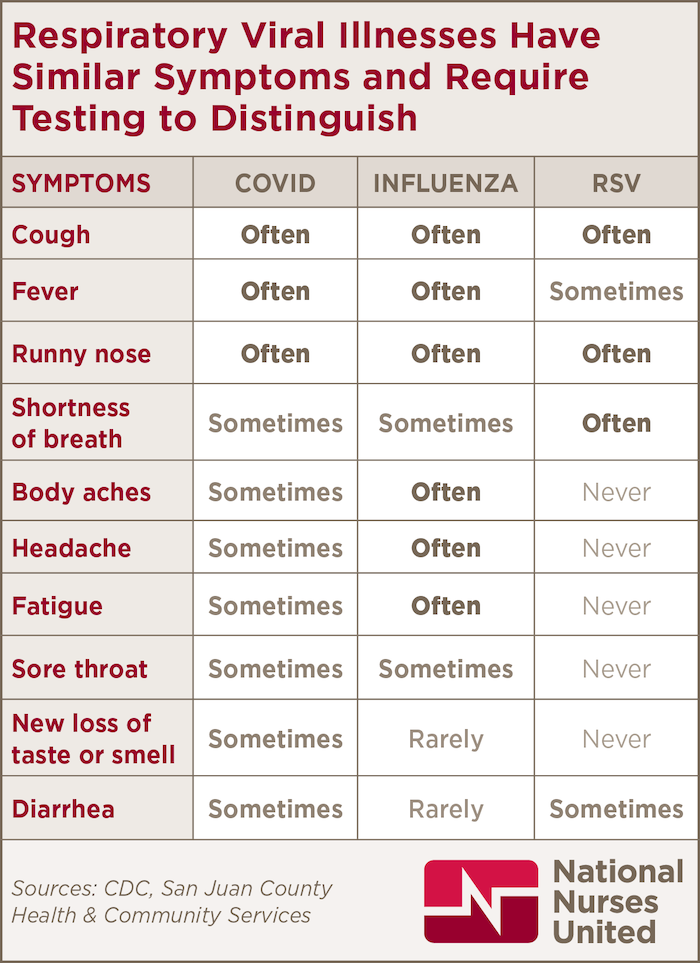
Workplace protections for nurses and caregivers must be based upon the scientific evidence and the precautionary principle, which states that we do not wait for proof of harm before taking action to protect people’s health. Based on symptoms alone, RSV, influenza, and Covid-19 are not easily distinguishable without a diagnostic test, and the science on transmission is very similar, indicating that they require similar protective measures.
- Hospitals should cancel non-urgent and elective surgical and other procedures in order to limit transmission of respiratory viral infections and to maintain capacity to respond to the surge in respiratory viral infections.
- Universal N95 use should be implemented for all staff when in contact with other staff, patients, and/or visitors. Other individuals, such as patients and visitors, should be required to wear a face covering.
- All patients and visitors should be screened for symptoms of a respiratory viral infection.
- Patients with symptoms of a respiratory viral infection should be isolated immediately. Diagnostic testing should account for the possibility of coinfections with SARS-CoV-2/Covid-19, influenza, and RSV.
- Visitors with symptoms or a recent diagnosis of a respiratory viral infection should be restricted from entering the facility.
- Designated cohort units should be created for patients with suspected/confirmed respiratory viral infections. Patients with different respiratory viral infections should not be placed in the same room.
- Cohorting of patients should be utilized. A nurse should never have both patients with suspected/confirmed respiratory viral infections and patients without respiratory symptoms/infections.
- Team nursing should not be utilized. Team nursing transgresses scopes of practices for registered nurses, licensed vocational nurses, and other health care personnel involved. Research clearly shows that team nursing results in poorer patient outcomes than primary nursing as it is prone to lead to role confusion and missed nursing care.
- Health care workers should be screened for respiratory symptoms prior to each shift and, if symptomatic, provided paid sick leave for missed work hours.
- Health care workers providing care to patients with suspected or confirmed respiratory viral infections should be provided with optimal personal protective equipment (PPE). Health care workers who perform screening of patients and visitors should also be provided with this PPE.
- A powered air-purifying respirator, but in no case should a health care worker be provided respiratory protection less protective than an N95 respirator.
- Eye protection
- Isolation gown
- Gloves
- Health care workers should be provided with prompt notification of exposures to respiratory viral infections. If a health care worker becomes symptomatic or tests positive for a viral respiratory illness following an exposure or possible exposure to an infected or potentially infected patient, coworker, or visitor, they shall be provided paid time off with no impact to their PTO or other benefits.
- Frequent environmental cleaning using disinfectants and cleaning chemicals that are effective against RSV, influenza, and SARS-CoV-2 in patient rooms and units where infected patients are placed and in common areas of the facility (e.g., lobbies, waiting rooms, stairwells, restrooms).
1. Hall, C.B., R.G. Douglas, et al., “Possible Transmission by Fomites of Respiratory Syncytial Virus,” J Infectious Diseases, 1980.
2. Bean, B., B.M. Moore, et al., “Survival of Influenza Viruses on Environmental Surfaces,” J Infectious Diseases, 1982.
3. Hirose, R., H. Ikegaya, et al., “Survival of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Influenza Virus on Human Skin: Importance of Hand Hygiene in Coronavirus Disease 2019 (COVID-19),” Clinical Infectious Diseases, 2021.
4. NNU, Droplet vs Airborne Fact Sheet.
5. Lindsley, W.G., F.M. Blachere, et al., “Distribution of Airborne Influenza Virus and Respiratory Syncytial Virus in an Urgent Care Medical Clinic,” Clinical Infectious Diseases, 2010.
6. Grimalt, J.O., H. Vílchez, et al., “Spread of SARS-CoV-2 in hospital areas,” Environ Res, 2022, https://doi.org/10.1016%2Fj.envres.2021.112074.
7. Bischoff, W.E., K. Swett, et al., “Exposure to Influenza Virus Aerosols During Routine Patient Care,” J Infectious Diseases, 2013.
8. Ferdinands, J.M., M.G. Thompson, et al., “Does influenza vaccination attenuate the severity of breakthrough infections? A narrative review and recommendations for further research,” Vaccine, 2021.
9. Behrouzi, B., D.L. Bhatt, et al., “Association of Influenza Vaccination With Cardiovascular Risk,” JAMA Network open, April 29, 2022, doi:10.1001/jamanetworkopen.2022.8873.
10. NNU Q&A Bivalent Boosters.