Professional and Patient Advocacy During the Omicron Surge

You can download a printable flyer with this information here.
Are you symptomatic?
According to the Centers for Disease Control (CDC), people with Covid-19 have had a wide range of symptoms – ranging from asymptomatic or mild symptoms to severe illness, regardless of vaccination or booster status.
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
A priority of registered nurses is to advocate for our patient's health, this includes advocating for our own health and safety. Nurses know the best way to protect our patients, ourselves, and preserve the integrity of the health care system amidst this infectious disease crisis is to advocate for the highest standards of care for our patients and for ourselves.
We want to protect patients, not infect them! If you think you have been exposed or are experiencing symptoms or have tested positive for Covid-19; trust your professional judgment. Call your primary care physician, call employee health, call infection control, file a workers' compensation claim with your employer, etc. Take the necessary steps to ensure you are doing your part to stop the spread.
How to protect yourself at work.
Omicron’s substantial immune evasive properties are resulting in high numbers of nurses and other health care workers contracting SARS-CoV-2 in their workplace, regardless of vaccination or booster status. A central component to all personal and professional decision-making is the precautionary principle. We are still learning about specific variables that might be unique to Omicron.1
Protect yourself at work by:
- Utilize universal airborne precautions irrespective of personal vaccination or booster status. Universal airborne precautions are recommended for direct-care nurses in all patient care settings
- Demand PPE (Personal Protective Equipment)! Protective PPE for nurses and other health care workers must include, at a minimum, N95 respirators or higher, isolation gowns, eye protection, and gloves in ALL patient care settings, irrespective of vaccination or booster status.

1 https://www.cdc.gov/coronavirus/2019-ncov/variants/omicron-variant.html
Scientific Brief: Post-Exposure Isolation Period for Omicron SARS-CoV-2 Variant
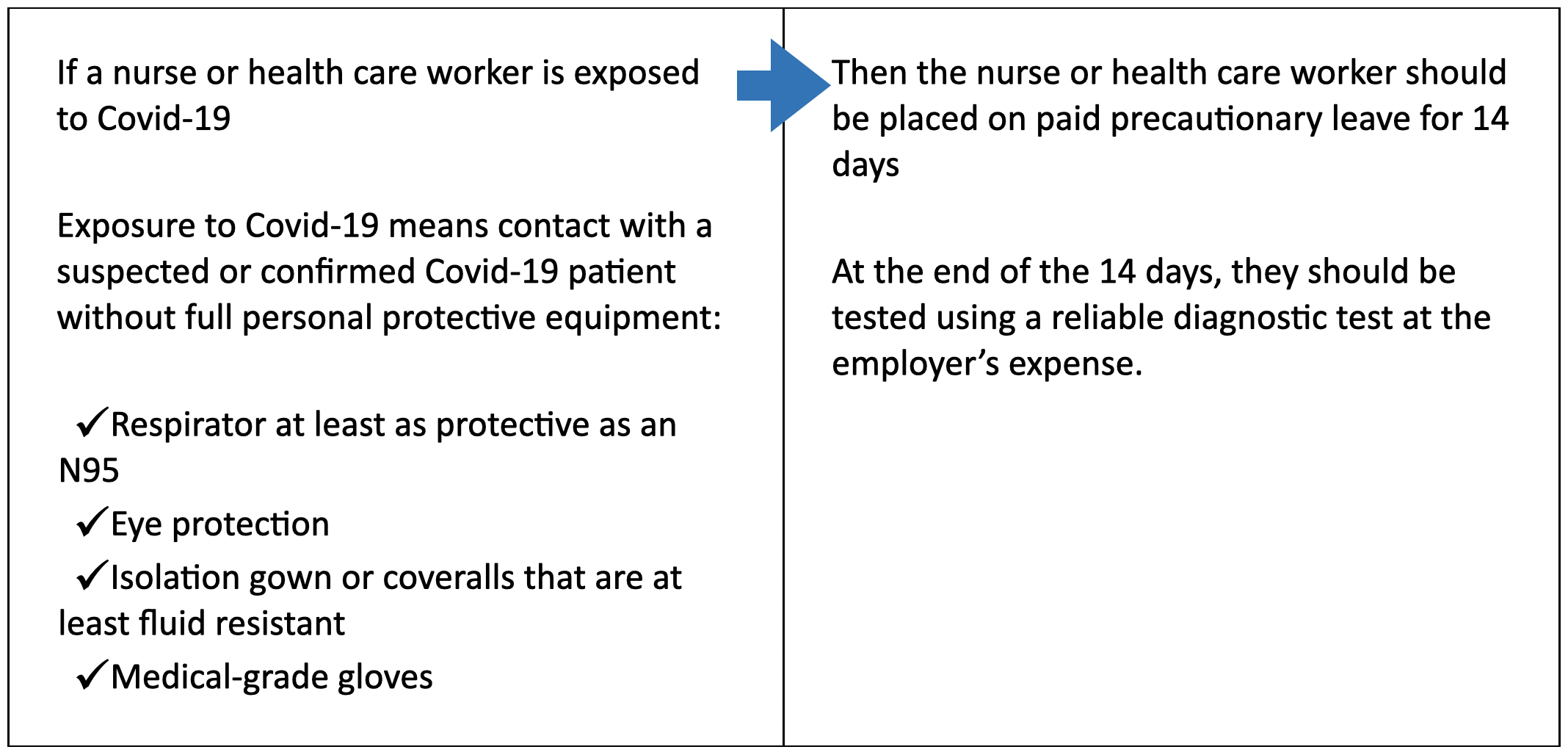
The incubation period for SARS-CoV-2, the virus that causes Covid-19, is 14 days. This is the amount of time after an exposure that it can take for an infection to develop.
While the average incubation period for the Omicron (B.1.1.529) SARS-CoV-2 variant is approximately three days,1,2 this is not an appropriate measure to use to determine the post-exposure isolation period. If the average incubation period is used to establish post-exposure isolation time periods, a significant proportion of cases will become infectious after that timeframe.
For public health and occupational health protection, it is necessary to use the range of incubation periods to ensure the timeframe effectively includes the majority of individuals. Research indicates the range of incubation period is approximately from one to fourteen days.3,4,5
The U.S. Centers for Disease Control and Prevention (CDC) recently shortened the isolation period for nurses and other workers who have tested positive for Covid-19 from 10 days to seven days and no longer require exposed vaccinated and boosted health care workers to quarantine.6 This guidance was updated “to limit the effects of staff shortages caused by Covid-19 on patient care.” In other words, there is no scientific basis from which this guidance was changed. A post-exposure period shorter than fourteen days will miss cases, leading to more transmission and endangering nurses, health care workers and their patients.
1 Brandal et al., “Outbreak caused by the SARS-CoV-2 Omicron variant in Norway to December 2021,” Eurosurveillance, December 15, 2021, Available at https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2021.26.50.2101147
2 Jansen et al., “Investigation of a SARS-CoV-2 B.1.1.529 (Omicron) Variant Cluster – Nebraska, November – December 2021,” MMWR Early Release, December 31, 2021, Available at https://www.cdc.gov/mmwr/volumes/70/wr/mm705152e3.htm
3 Yan, Lin, Jingyi Dai, et al., “Estimation of incubation period and serial interval of COVID-19: analysis of 178 cases and 131 transmission chains in Hubei province, China,” Epidem & Infect, June 19, 2020.
4 Tan, W.Y.T., L.Y. Wong, et al., “Does incubation period of COVID-19 vary with age? A study of epidemiologically linked cases in Singapore,” Epidem & Infect, Sept 2, 2020.
5 Elias, C., Sekri, A., Leblanc, P., Cucherat, M., & Vanhems, P. (2021). The incubation period of COVID-19: A meta-analysis. International Journal of Infectious Diseases, 104, 708-710. https://doi.org/https://doi.org/10.1016/j.ijid.2021.01.069
6 U.S. Centers for Disease Control and Prevention, “Interim Guidance for Managing Healthcare Personnel with SARS-CoV-2 Infection or Exposure to SARS-CoV-2,” December 23, 2021, https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html
More Resources
Droplet Vs. Airborne: How Is Sars-cov-2 Transmitted?
The U.S. Centers for Disease Control and Prevention (CDC) states that the primary mode of transmission for Covid-19 is droplet transmission and that “airborne transmission from person-to-person over long distances is unlikely.”
The Covid Exposure Blame Game
Since the beginning of the Covid-19 pandemic, nurses and health care workers have called for employers and governments to follow the precautionary principle — that we shouldn’t wait for proof of harm before implementing measures to protect health.
Growing scientific research affirms the need for comprehensive infection control plans and optimal PPE to prevent transmission of Covid-19 within health care facilities. But employers continue to neglect basic infection control measures and, instead, are blaming nurses.
Reuse of N95 respirators endangers nurses, health care workers, and their patients
A study confirms: N95s donned more times and worn for more hours were more likely to fail fit-tests — meaning these N95s did not seal to the wearers’ faces and failed to provide the minimum level of protection.
Extended use and reuse of N95s led to high rates of fit-test failure. N95s were designed for single use only!