Press Release
Mission HCA RNs Protest Unsafe Staffing as COVID-19 Cases Surge
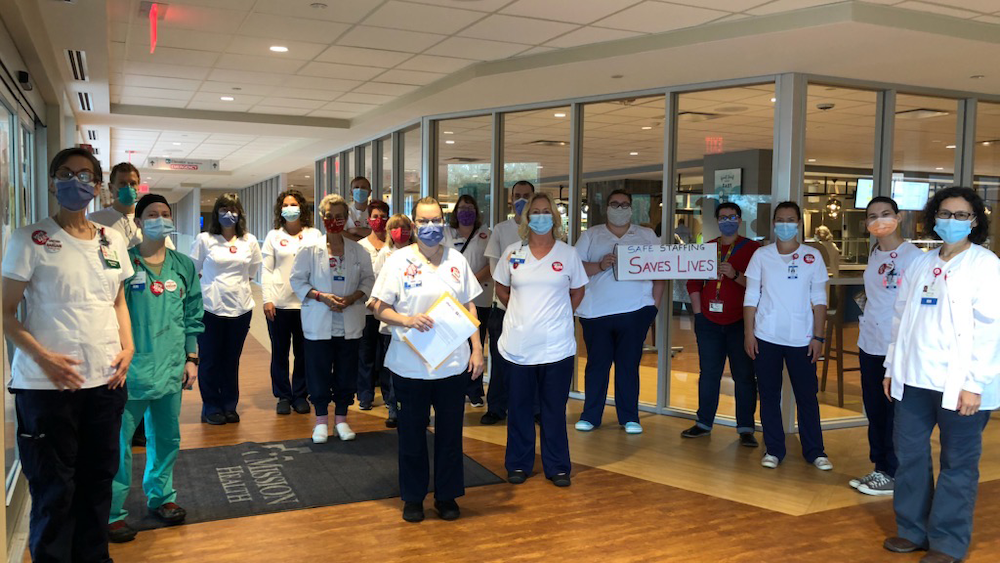
Registered nurses at HCA’s Mission Hospital in Asheville, NC are marching on the hospital’s chief executive this morning to protest what they see as an alarming rise in unsafe staffing at the very moment the hospital is swamped with COVID-19 patients.
“Nurses at Mission are organizing to ensure that the Western North Carolina Community receives the highest standard of care possible. However, currently, conditions at the hospital are such that patient care is suffering,” the letter to hospital administration says. “Furthermore, the Covid-19 pandemic has exacerbated all existing issues and we are on the verge of a local healthcare crisis if steps to alleviate the situation are not immediately taken.”
(RN interviews will be available after the morning action by calling 240-460-0352)
The Mission RNs are demanding the hospital hire additional full and part-time RNs and support staff to immediately address what they call dangerous short staffing that puts patients at risk.
To make conditions worse, the staffing shortages occur as patients infected with the coronavirus are arriving in the hospital in record numbers, concurrent with the pandemic surge across the state. Some two-dozen confirmed COVID-19 patients are currently at Mission, with about 20 other suspected cases awaiting test results.
“With the pandemic and the increase of cases in the hospital, the risk of exposure and infection is growing as nurses rush to take care of patients without the backup of additional staff. The pressures of providing care with inadequate staffing does not allow for the time needed to ensure we do not make mistakes which is not acceptable,” said Jill Rabideau, a float pool RN at Mission.
“These are very dangerous conditions. We are insisting that the hospital administration act immediately to protect nurses, all hospital staff, patients, and the community,” said Kelley Tyler, a Trauma Care Unit RN at Mission.
Among other demands, the nurses are calling on the hospital to determine staffing assignments on the basis of acuity – the actual severity of each patient’s illness – rather than artificial, budget-based staffing grid numbers, as well as increased transparency about staffing that is available to the nurses.
“When we do not have enough RNs at the bedside, we are not able to give our patients the essential, individual care they need when they are at their most vulnerable,” said Trish Stevenson, an Emergency Department RN. “It is heartbreaking for our patients, and unconscionable for our frontline staff.”
The emergency department, which is also where COVID-19 patients arrive, has been flooded with patients with RNs expect to care for multiple patients at a time, some of who should be receiving more intensive care.
“There are patients who are suddenly seizing, and you just don’t have the resources to deal with any kind of emergent situation in intake. But you can’t rush them to a bed because you have 12 other patients and there might not even be a bed available,” says one ER RN.
Poor staffing is especially serious in psychiatric care units, which has led to increased incidents of workplace violence “on a regular basis when understaffed” with a number of injuries to staff and patients, one Psychiatric RN reports.
In addition, while the hospital began virus testing before admitting patients, “they are admitting high risk patients who refuse the COVID-19 test potentially infecting the patients and staff on the unit,” says another Psychiatric RN.
Trauma Care Unit RNs also report excessive patient admissions with not enough staff. In one representative case, a TCU RN reports, she had to spend a lot of extra time with one very ill patient “and it put my other people in potentially dangerous situations. On top of that I had other patients who still needed monitoring, medication and changing. It was not possible to do everything.”