National Nurses United’s Standards for Hospital Safety During the Covid-19 Pandemic
Two years into the Covid-19 pandemic, the SARS-CoV-2 variants of concern like Delta and Omicron have caused Covid cases to surge in communities throughout the United States. Hospitals and other health care facilities have continued, even until now, to put registered nurses and other health care workers at risk by not providing safe patient care conditions. As a result, nurses and other health care workers have faced staggering rates of infections and deaths.
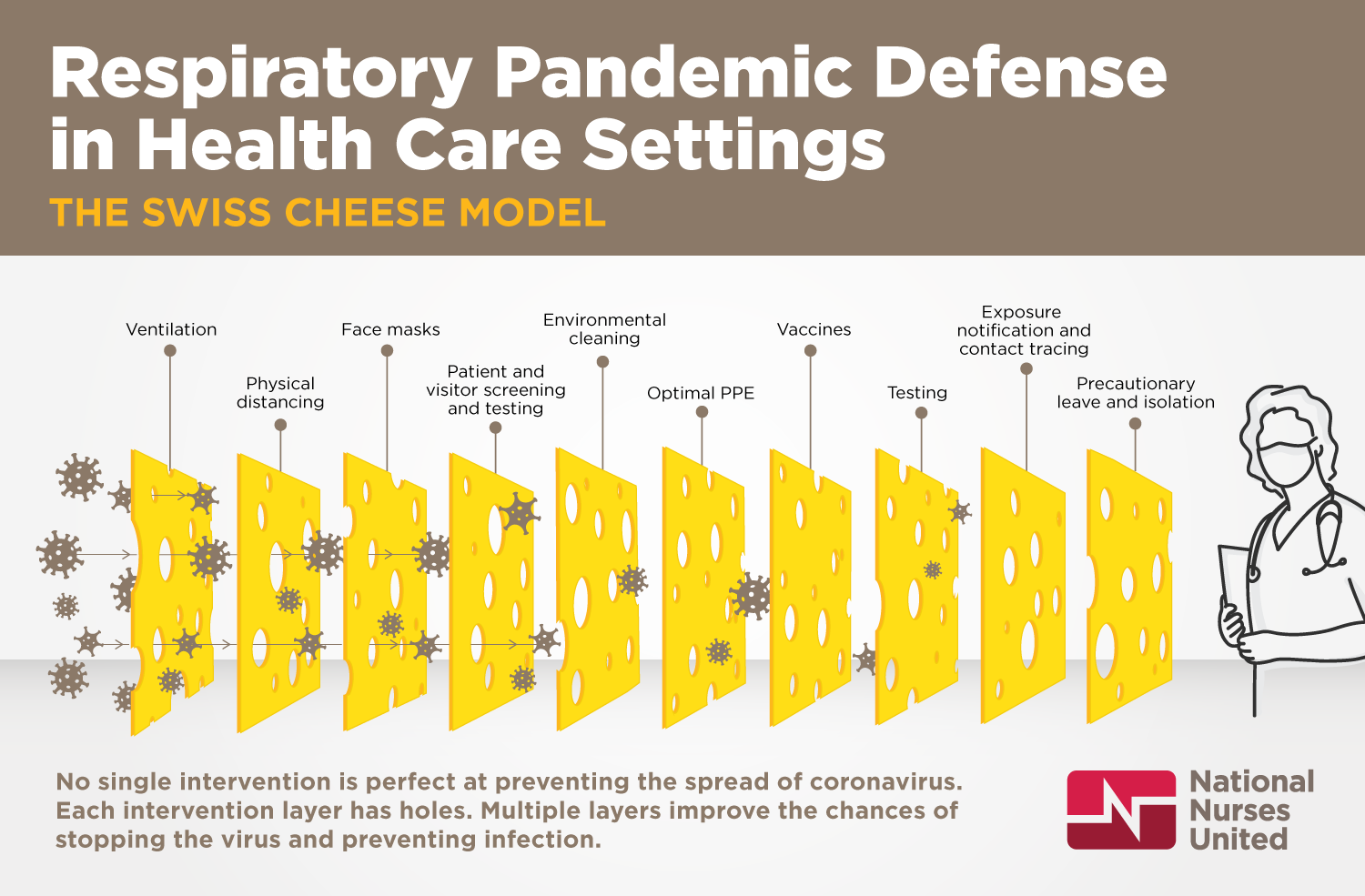
Hospitals and other health care facilities have a duty to ensure a safe environment for staff and patients. During the Covid-19 pandemic, hospitals and other health care facilities should implement the following protective measures to prevent transmission of SARS-CoV-2 within their facilities:
- COVID-19 VACCINES Employers should make Covid-19 vaccines, including boosters, readily available and accessible to all employees, at no cost. Surveillance testing, isolation, precautionary leave, respiratory protection, and other PPE should remain in place, irrespective of vaccination status. Covid-19 vaccines are one important element, but by themselves are not enough to combat this pandemic. Preventing SARS-CoV-2 transmission while increasing vaccination must happen concurrently to maintain the current level of protection that Covid vaccines provide. Failure to prevent widespread transmission will result in further evolution and spread of variants of concern that evade vaccine protection.
- PATIENT SCREENING All patients should be considered possible Covid-19 cases until confidently ruled out as non-Covid-19 patients or confirmed as Covid-19 patients, irrespective of vaccination status. Hospitals must screen all patients using a combination of testing, symptom screening, and epidemiologic history. Since vaccinated patients may still be able to transmit the virus, this screening should be done regardless of vaccination status or in addition to verification of vaccination status. Patients should then be directed to the appropriate zones of the facility (see next bullet point). Hospitals cannot rely solely on testing or symptom screening to identify Covid-19 patients because asymptomatic/pre-symptomatic cases are a significant source of transmission, and testing is often unreliable. Any exposure history (e.g., contact with a Covid-19 case, recent travel, or other possible exposure) should be considered when assigning patients to a designated area. Even with a negative diagnostic test, some patients should be classified as possible Covid-19 cases either due to symptoms or recent exposure.
- SEPARATE, DESIGNATED ZONES for confirmed Covid-19 patients, possible Covid-19 patients, and non-Covid-19 patients. Facilities must establish three separate zones to prevent transmission of the virus within the facility: (1) Covid zone: Confirmed Covid-positive patients should be cared for in designated area(s) to reduce the possibility of transmission of the virus to other patients. (2) Potentially infectious zone: Possible Covid-19 patients should be cared for in a designated part of the facility with appropriate precautions in place to prevent transmission of the virus. All patients who have not yet been confirmed Covid-positive or ruled out as non-Covid patients should be cared for in this zone. (3) Non-Covid zone: A separate non-Covid area should be established to care for patients who have been ruled out as non-Covid patients using testing, symptom screening, and exposure history. When non-Covid patients are mixed with confirmed Covid patients and possible Covid-19 patients, the potential for transmission of the virus to both staff and patients increases significantly. Separate areas are necessary in all areas of the hospital, including inpatient units, emergency departments, labor and delivery, and procedural areas.
- ISOLATION ROOMS AND VENTILATION Confirmed and possible Covid-19 patients should be placed in airborne infection isolation rooms (AIIRs). These AIIRs reduce the possibility that infectious viral particles will be transported to other areas of the facility. Facilities should also consider converting additional rooms, units, and floors with confirmed and possible Covid-19 patients to negative pressure.
- OPTIMAL PERSONAL PROTECTIVE EQUIPMENT (PPE) Nurses and other health care workers who are providing care or who have contact with confirmed and possible Covid-19 patients should have optimal PPE, irrespective of vaccination status. Optimal PPE for Covid-19 includes a powered air-purifying respirator (PAPR), coveralls that are impervious to viral penetration, head and shoe coverings, and gloves.
Under no circumstances should nurses and other health care workers be provided less than minimal PPE for Covid-19: single-use N95 filtering facepiece respirator, eye protection (goggles or face shield), isolation gown, and gloves. Single-use N95 filtering facepiece respirators should not be reused or decontaminated; these are dangerous practices that increase the risk of transmission to staff and patients.
If a health care facility cannot acquire enough N95 filtering facepiece respirators to meet need, then they should use respirators designed to be reusable, including PAPRs and elastomeric respirators. - STAFFING Health care facilities should ensure safe staffing at all times. Patient assignments should not include both Covid-positive and non-Covid-19 patients; mixed assignments increase the potential for transmission of the virus between patients and staff. Where health care workers must wear PPE for long periods of time, frequent breaks should be provided to prevent fatigue and skin injuries.
- STAFF EXPOSURES Health care facilities should proactively monitor and prevent all staff exposures to Covid-19. Exposure includes any time staff has contact with a patient and is not wearing full PPE (respirator, eye protection, coveralls or gown, and gloves). Any time staff is exposed to the virus, they should be placed on paid precautionary leave for at least 14 days. Staff should be notified as soon as possible if they have been exposed.
- TESTING Testing should be made readily available to nurses without cost. Nurses and other health care workers must be able to get tested regardless of vaccination status, or whether they have developed symptoms or remain asymptomatic.
- REMOVAL OF PRECAUTIONS FOR PATIENTS Precautions should only be removed when a Covid-19 patient has been confirmed to be no longer actively shedding virus and no longer potentially infectious. The Centers for Disease Control and Prevention (CDC) recommends removing precautions 10 days after symptoms began. There is not yet scientific certainty about the timeframe in which Covid-19 patients are infectious. If precautions are removed too early and the patient is still infectious, the consequences can be severe. Therefore, precautions should be maintained for patients until they are confirmed to no longer be shedding virus (e.g., have at least two negative tests 24 hours apart).
- RETURN-TO-WORK FOR POSITIVE STAFF Staff who have tested positive for Covid should return to work after their symptoms, if any, have resolved and after they have received two negative tests at least 24 hours apart. Due to the possibility of recurrent positives, employers should provide ongoing testing for positive staff at least weekly. There is increasing evidence of the significant role that asymptomatic infections play in transmission. Therefore, asymptomatic positive staff should not be treated differently from symptomatic positive staff.
- MEASURES TO PREVENT INTRODUCTION OF VIRUS TO THE FACILITY Employers should implement additional measures to prevent introduction of the virus to the facility. These measures include visitor restrictions, visitor screening, universal source control (all staff, patients, visitors, and others present in the facility should wear a surgical or cloth mask to reduce their respiratory emissions), frequent and thorough environmental cleaning, and paid sick and family leave for staff.
- PROCEDURAL AND OUTPATIENT AREAS Hospitals reopening procedural areas should have all of these safety precautions in place to prevent transmission within the facility and to protect nurses, other health care workers, and patients from exposure. If a hospital is unable to implement all of these safety precautions (e.g., they are reusing N95 respirators), then the hospital should delay elective procedures.
FOR MORE INFORMATION:
NNU’s Covid-19 Resources Webpage
NNU’s Model Standards for Covid-19 Surge
NNU’s Safety Requirements for Hospitals Reopening Procedural and Outpatient Areas
NNU’s Covid Testing and Screening in Health Care Settings
NNU Scientific Brief: Post-Exposure Isolation Period for Covid-19
NNU’s PPE Decontamination Statements and Materials