Mpox: What nurses need to know
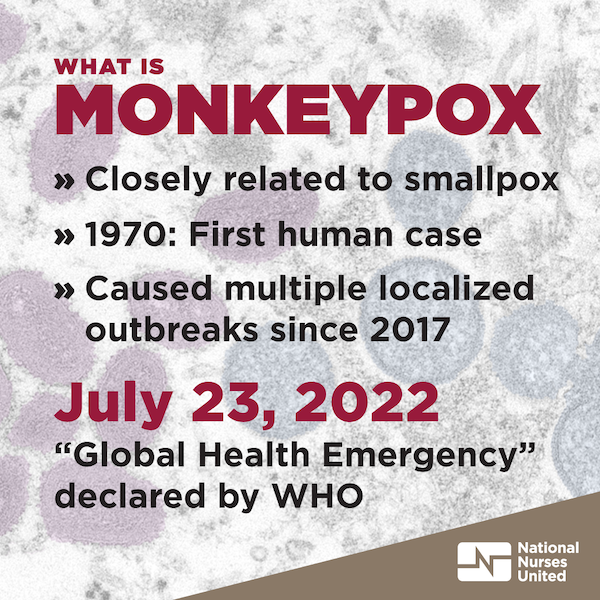
What is mpox (monkeypox)?
Human mpox is a zoonotic viral disease caused by the mpox virus, which belongs to the same family of viruses as smallpox. The first human case was identified in 1970.1 Mpox is considered a re-emerging disease that has caused multiple localized outbreaks since 2017. On November 28, 2022, the World Health Organization officially renamed the monkeypox virus disease as mpox2 in an effort to avoid racist, stigmatizing and othering of certain populations.
There are two clades of mpox: Clade I (with subclades Ia and Ib) causes more severe illness with up toa 10 percent mortality rate and Clade II causes less severe illness and 99.9 percent of people survive. In 2022, mpox (Clade II) began spreading rapidly in many countries that have not historically had cases. While cases have declined in some countries since then, the current mpox outbreak in the United States is not over. In 2024, a novel mpox lineage (termed Clade Ib) began surging again in several countries in Africa and the World Health Organization (WHO) declared the outbreak a public health emergency of international concern.3,4
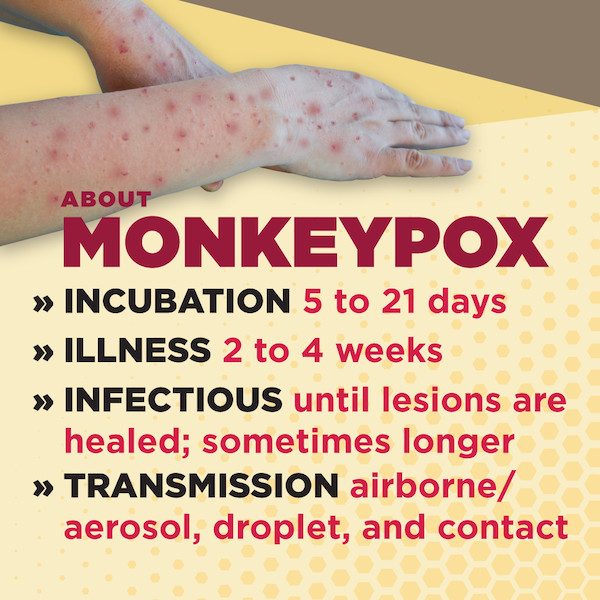
About the virus:
- Incubation period ranges from 5 to 21 days.
- Illness typically lasts for 2 to 4 weeks.
- Infectious period lasts until all scabs or crusts have fallen off, though may extend longer for some individuals.
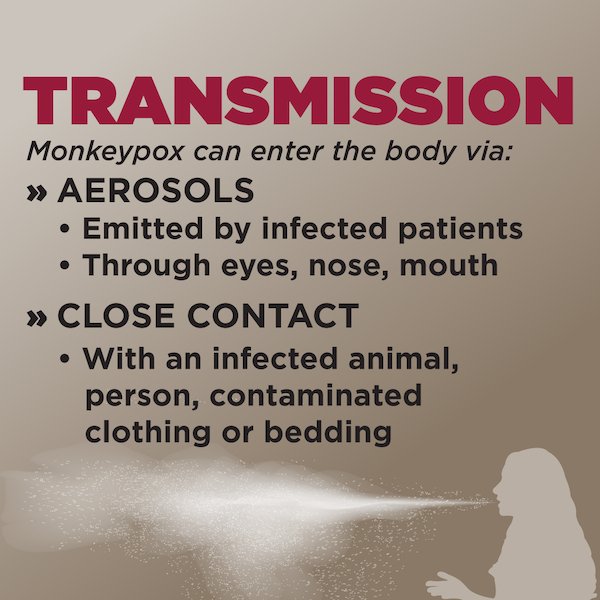
- Transmission modes include airborne/aerosol, droplet, and contact.
What are the symptoms and complications of mpox?
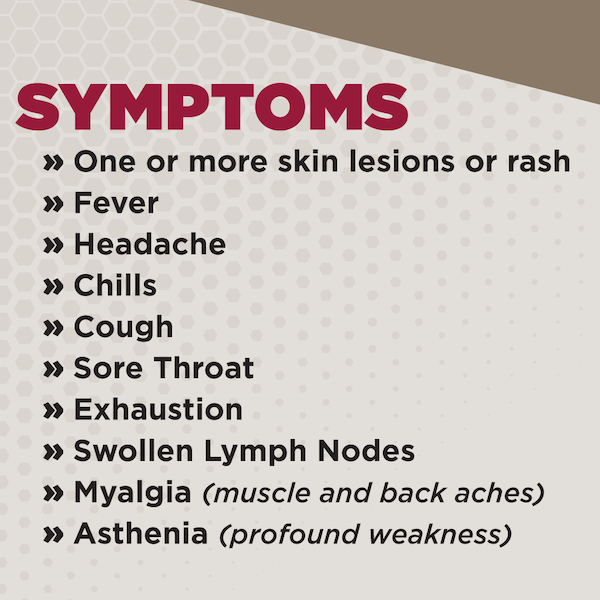
Mpox can have wide-ranging clinical manifestations, including:
- Rash or skin lesion on the face, inside of the mouth, hands, feet, chest, and other parts of the body. Skin lesions may vary in size and range from a few to several thousand and may look like pimples or blisters. NOTE: many people in the current outbreak present with only one single lesion.5
- Fever
- Headache
- Chills
- Cough
- Sore throat
- Exhaustion
- Swollen lymph nodes
- Myalgia (muscle and backaches)
- Asthenia (profound weakness)
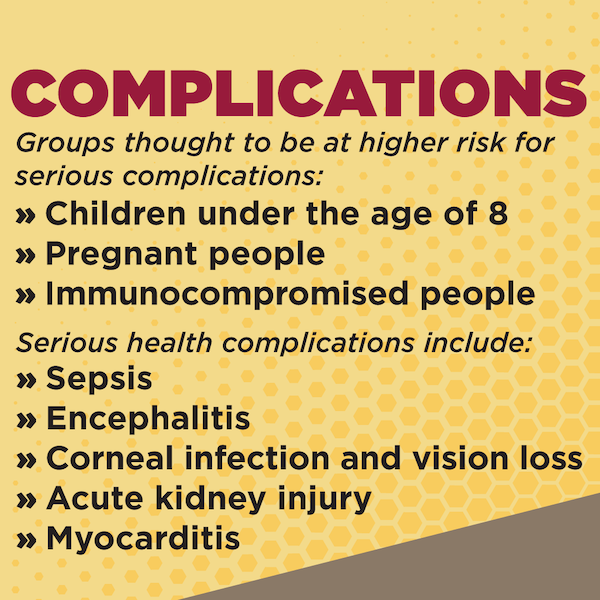
While mpox is usually self-limiting and typically spontaneously resolves within a few weeks, some individuals (e.g., children, pregnant women, and immunocompromised persons) may experience serious health complications including:6
- Sepsis
- Encephalitis
- Secondary infections
- Bronchopneumonia
- Abscess and airway obstruction
- Corneal infection and vision loss
- Myocarditis
- Acute kidney injury
How is mpox transmitted?
Human-to-human mpox transmission, including nosocomial and household transmission, has been well documented. Mpox can be transmitted through close contact with an infected animal (e.g., rodents) or human, or fomites (e.g., contaminated clothing or bedding) and through infectious aerosols emitted by patients in the infectious period. The virus can enter the body through the respiratory tract, broken skin (even if not visible, via contact with bodily fluids), or mucous membranes (eyes, nose, or mouth).
Prolonged upper respiratory tract viral shedding from patients with mpox has been documented even after skin lesion resolution.7 Transmission from viral shedding may also begin prior to the onset of rash.8
Asymptomatic cases have been documented, with some studies estimating up to 14 percent of cases.9,10
What protections do nurses and other health care workers need to care for a patient with confirmed or suspected mpox?
Mpox requires airborne, contact, and droplet precautions.
- Suspected or confirmed mpox cases must immediately be placed in airborne infection isolation rooms (also called a negative pressure room).
- Nurses and other health care workers should have the highest level of personal protective equipment (PPE) when caring for patients with suspected or confirmed mpox.
- Highest level of PPE for mpox: powered air-purifying respirator (PAPR), coveralls impermeable to viral penetration that incorporate head and shoe covering, and gloves.
- Minimum level of PPE for mpox: fit-tested, single-use N95 respirator, isolation gown, goggles, and gloves.
- Infectious mpox virus can be resuspended in aerosols when contaminated objects (e.g., bedding, clothing, or PPE) are shaken or moved. Mpox virus particles have been found to retain infectivity in aerosols from 18 to 90 hours.11
- Strict procedures for donning and doffing PPE upon entry and exit from the patient’s isolation room must be followed.
- Cleaning protocols must be observed after each doffing for PPE designed to be reused (e.g., PAPRs).
- Tight control of patient transport and health care worker movement through the facility must also be implemented to prevent transmission or contamination of mpox.
NOTE: For nurses who work in California, the Cal/OSHA Aerosol Transmissible Diseases Standard requires that health care facilities implement airborne precautions for mpox cases, including:
- Placement of patients with suspected or confirmed mpox in a negative pressure room.
- Use of an N95 or more protective respirator, in combination with other required PPE (gown, gloves, eye protection) for any encounter with a patient with suspected or confirmed mpox.
- Use of a PAPR for aerosol-generating procedures performed on patients with suspected or confirmed mpox.
1. Ježek et al., “Human Monkeypox: Clinical Features of 282 Patients,” The Journal of Infectious Diseases, August 1987
2. U.S. Centers for Disease Control and Prevention, “CDC Changes Monkeypox Terminology to Mpox,” November 28, 2022
3. World Health Organization, “WHO Director-General declares mpox outbreak a public health emergency of international concern,” August 14, 2024
4. Vakaniaki et al., “Sustained human outbreak of a new MPXV clade I lineage in eastern Democratic Republic of the Congo,” Nature Medicine, June 13, 2024
5. U.S. Centers for Disease Control and Prevention, “Clinical Recognition: Key Characteristics for Identifying Mpox,” last updated August 30, 2023
6. Thornhill, J.P., S. Barkati, et al., “Monkeypox Virus Infection in Humans across 16 Countries — April–June 2022,” NEJM, July 21, 2022
7. Adler et al., “Clinical features and management of human monkeypox: a retrospective observational study in the UK,” The Lancet Infectious Diseases, May 2022
8. Nolen et al., “Extended Human-to-Human Transmission during a Monkeypox Outbreak in the Democratic Republic of the Congo,” Emerging Infectious Diseases, June 2016
9. Hammurland et al., “Multiple diagnostic techniques identify previously vaccinated individuals with protective immunity against monkeypox,” Nature Medicine, August 2005
10. Rossotti et al., “Detection of Asymptomatic Mpox Carriers among High-Ri Men Who Have Sex with Men: A Prospective Analysis,” Pathogens, June 2023
11. Verreault, Daniel et al. “Susceptibility of monkeypox virus aerosol suspensions in a rotating chamber,” Journal of Virological Methods, February 2013