Blog
'Treat us better': Nurses flee hospital jobs because working conditions aren't safe
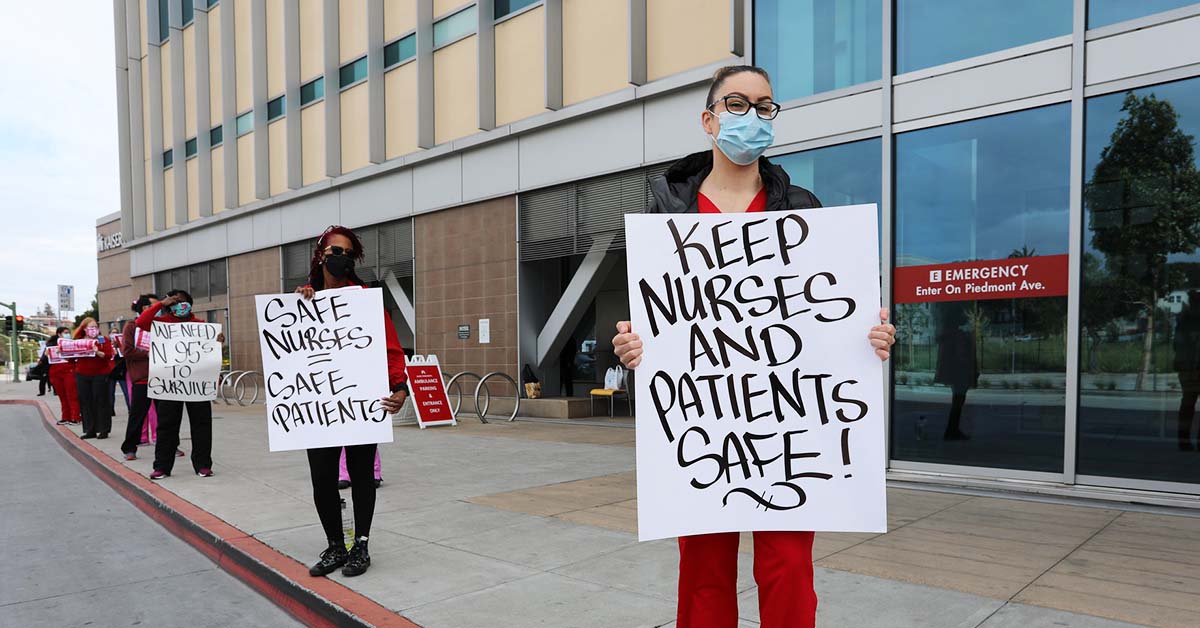
Nurses are unwilling to risk their licenses or their patients’ lives by working in unsafe conditions.
Listening to hospital executives lament the "nursing shortage" is beyond infuriating.
Nurses know the United States is not feeling a true nursing shortage, only a shortage of nurses willing to risk their licenses or their patients’ lives by working in unsafe conditions.
Except for a few states, plenty of registered nurses are available to meet this country’s needs, according to a 2017 U.S. Department of Health and Human Services report on the supply and demand of the nursing workforce from 2014 to 2030.
Some states will even have too many. But when hospitals understaff units and shifts to maximize profits – leaving nurses with morally distressing choices about how to allocate care – it’s no surprise many of us make the difficult decision to leave.
“The hospital keeps saying, ‘We appreciate you,’ but we are not seeing any action,” said Maggie Webb, a registered nurse at the University of Chicago Medical Center's pediatric intensive care unit.
She will lose half a dozen colleagues in the coming weeks, as poor working conditions drive nurses away.
“We are basically being told to just grin and bear it, and hope for the best – and hopefully nothing bad happens to our patients," Webb said. "That’s not fair to them. This is our livelihood, this is our lives, and we are putting our nursing licenses at risk because of staffing.”
Bare-bones staffing even before Covid
Long before the pandemic, hospitals staffed at bare-bone levels to maximize profit, rather than at the level needed to safely care for patients and the severity of their conditions.
The pandemic took the unsafe staffing to nightmare levels.
In late August, registered nurses in the emergency department at Northside Hospital in St. Petersburg, Florida, reported shifts with more than 20 patients assigned to one staff nurse and one charge nurse (who should be a resource, not have a full patient load).
“We sometimes have patients overflowing the lobby, waiting ridiculous hours to be triaged, examined and treated. But we have to fight every step of the way to get the hospital to staff up for these patients,” said Mawata Kamara, an emergency department registered nurse at San Leandro Hospital in San Leandro, California.
Employers often act like nurses are interchangeable cogs, regardless of our area of expertise. At Research Medical Center in Kansas City, Missouri, medical/surgical nurses report being overwhelmed with six patients at once, some of them too critical for that unit.
“A lot of these patients, we don't have the expertise to care for on my floor, let alone when they're one of six patients,” said research RN Zoe Schmidt. “It has happened multiple times that nurses, and even doctors, have expressed concern about patients needing a higher level of care than my unit, only to be told by the house supervisor that there's no open beds anywhere else.”
Since Day One of Covid-19, nurses have told our managers to prepare for predictable staffing needs, including hiring and training more nurses, and cross training nurses to work in critical care departments. They didn’t listen.
Our employers play games with their available staffing pool to slash labor costs – including sending nurses home who have reported for their shifts, canceling nurses who are scheduled to work on a daily contract basis, laying off staff from units with a temporarily low patient census, canceling traveling nurse contracts, and failing or being extremely slow to hire for open positions.
In states where it’s still allowed, our employers also impose mandatory overtime on nurses.
Nurses faced with impossible choices
When employers force us to make impossible choices between patients, during 12-hour shifts with no time to eat or use the bathroom, is it any wonder nurses leave?
We have a simple, effective solution for encouraging nurses to return to providing the direct patient care we desperately need during this pandemic: Treat us better!
Ensure safe working conditions, including enough staff on every shift, and implement all the measures of infection control that we need to protect ourselves and our patients.
Meanwhile, don’t pretend the staffing crisis was inevitable or unavoidable due to Covid-19. Hospitals manufactured this crisis.
Bonnie Castillo, a registered nurse, is executive director of National Nurses United, the largest union of registered nurses in the United States, with more than 175,000 members.