The science of ratios

Decades of studies have shown that more nurses equate to lives saved and fewer complications. After ratios were implemented in California, research demonstrated that ratios were working! Now that that relationship has been well established, researchers have been focusing on what exactly is the mediating link between increasing RN staffing and improved outcomes. It’s no surprise to us that, once again, the most recent studies are echoing what nurses have always said, “Care is being left undone.” In other words, “missed” nursing care. Ratios lower the patient assignment load for nurses so that they do have the time, energy, and capacity to actively provide this care that makes all the difference.
What follows below is a review of the most important studies that have been conducted and published about ratios, loosely grouped into categories. Due to the nature of academic research which often examines only a facet of a subject or topic, it is hard to make sweeping generalizations about the cause and effect of safe staffing ratios, but all signs point to the benefits of ratios.
Saving lives!
A study of more than 11,000 patients over a two-year period in 75 hospitals in four states across the country (Pennsylvania, New Jersey, Florida, and California) found that “better work environments and lower patient-to-nurse ratios on medical-surgical units were associated with increased odds of survival after in-hospital cardiac arrest, even after taking into account other likely explanations. The likelihood of survival was 16 percent lower for patients cared for in hospitals with poor nursing work environments. In addition, the odds of survival were 5 percent lower for each additional patient per nurse on medical-surgical units.”
--McHugh, M. D., et al. American Heart Association’s Get With The Guidelines-Resuscitation, I. (2016). Better Nurse Staffing and Nurse Work Environments Associated With Increased Survival of In-Hospital Cardiac Arrest Patients. Med Care, 54(1), (pp. 74-80) Retrieved August 14, 2018 from doi:10.1097/MLR.0000000000000456
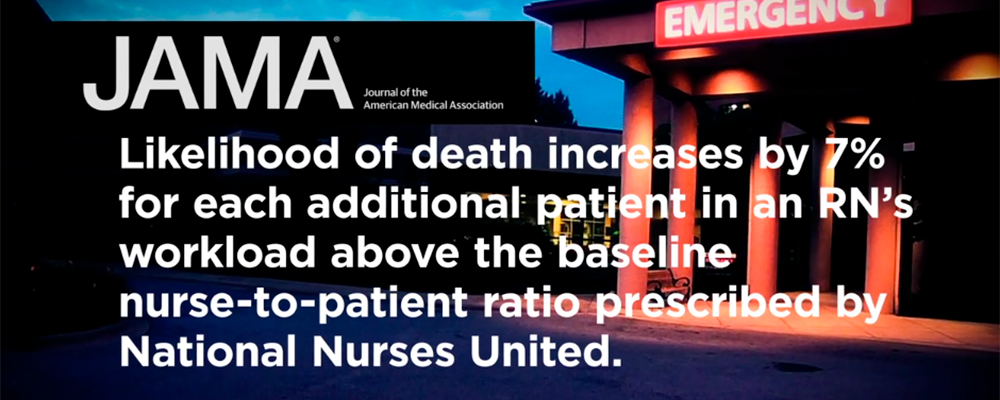
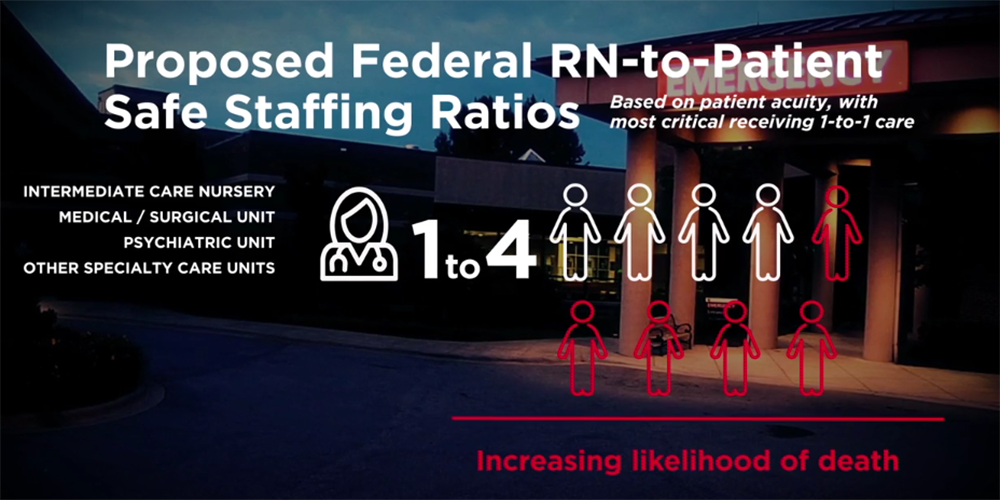
The odds of patient mortality increased by 7 percent for every additional patient in the average nurse’s workload in the hospital and that the difference from four to six and from four to eight patients per nurse would be accompanied by 14 percent and 31 percent increases inmortality, respectively.
--Aiken, L. H.; Clarke, S. P.; Sloane, D. M.; Sochalski, J.; & Silber, J. H. (2002) Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA, 288(16), (1987-1993) Retrieved August 14, 2018 from doi:10.1001/jama.288.16.1987
When emergency nurses cared for three additional patients in 24 hours, the time to diagnostic evaluation in trauma emergency departments doubled from approximately half an hour to one hour, and in non-trauma emergency departments, time to diagnostic evaluation increased by approximately 15 minutes.
--Shindul-Rothschild, J.; Read, C. Y.; Stamp, K. D.; & Flanagan, J. (2017) Nurse Staffing and Hospital Characteristics Predictive of Time to Diagnostic Evaluation for Patients in the Emergency Department. Journal of Emergency Nursing, 43(2), (pp. 138-144) Retrieved August 14, 2018 from doi:10.1016/j.jen.2016.07.003
Nurses from units with low staffing and poor organizational climates were twice as likely as nurses on well-staffed and better-organized units to report risk factors for needlestick injuries and near misses.
--Clarke, Sloane, & Aiken, 2002
Substantial NICU nurse understaffing relative to national guidelines is widespread. Understaffing is associated with an increased risk for VLBW nosocomial infection.
--Rogowski, J. A., et al. (2013) Nurse staffing and NICU infection rates. JAMA Pediatrics, 167(5), (pp. 444-450) Retrieved August 14, 2018 from doi:10.1001/jamapediatrics.2013.18
Our findings suggest that the most vulnerable hospitalized patients, unstable newborns requiring complex critical care, do not receive recommended levels of nursing care. Even in some of the nation’s best NICUs, nurse staffing does not match guidelines.
--Rogowski, J. A., et al. (2013) Nurse staffing and NICU infection rates. JAMA Pediatrics, 167(5), (pp. 444-450) Retrieved August 14, 2018 from doi:10.1001/jamapediatrics.2013.18
Each additional patient per nurse is associated with 12% higher odds of in-hospital mortality, 7% higher odds of 60-day mortality, 7% higher odds of 60-day readmission, and longer lengths of stay, even after accounting for patient and hospital covariates including hospital adherence to SEP-1 bundles.
--Karen B. Lasater PhD, RN; Douglas M.Sloane PhD; Matthew D.McHugh PhD, RN, FAAN; Jeannie P.Cimiotti PhD, RN, FAAN; Kathryn A.Riman BSN, RN; Brendan Martin PhD; Maryann Alexander PhD, RN, FAAN; Linda H.Aiken PhD, RN; et al. Evaluation of hospital nurse-to-patient staffing ratios and sepsis bundles on patient outcomes. (2021)
Nurse staffing on medical and surgical units in Illinois hospitals averaged 5.4 patients per nurse and ranged from as few as 4.2 patients per nurse to as many as to 7.6. These estimates suggest that few Illinois hospitals are currently meeting the minimum staffing levels which would be required by the Safe Patient Limits Act currently under consideration. We found that each additional patient in a nurses’ workload was associated with 16% higher odds of death and longer lengths of stay. If Illinois hospitals staffed medical and surgical units at the ratio proposed in the legislation, we project thousands of deaths could be avoided each year and patients would experience shorter lengths of stay resulting in hundreds of millions of dollars in cost-savings for hospitals.
--Karen B Lasater; Linda H Aiken; Douglas Sloane; Rachel French; Brendan Martin; Maryann Alexander; Matthew D McHugh; et al. Patient outcomes and cost savings associated with hospital safe nurse staffing legislation: an observational study. (2021)
Protecting patients 24/7
In New Jersey, weekend presentation to the ED with a diagnosis of acute myocardial infarction was associated with an increase in patient mortality. Investigators recommend that nurse staffing should continue to remain consistent across all the days of the week.
--de Cordova, P. B.; Johansen, M. L.; Martinez, M. E.; & Cimiotti, J. P. (2017) Emergency Department Weekend Presentation and Mortality in Patients With Acute Myocardial Infarction. Nursing Research, 66(1), (pp.20-27) Retrieved August 14, 2018, from doi:10.1097/nnr.0000000000000196
A national study on the rate of death from cardiac arrest in hospitals found that the risk of death from cardiac arrest in the hospital is nearly 20 percent higher on the night shift. The authors highlight understaffing during the night shift as a potential explanation for the death rate. “Most hospitals decrease their inpatient unit nurse-patient ratios at night. Lower nurse-patient ratios have been associated with an increased risk of shock and cardiac arrest.”
--Peberdy, M. A., et al. National Registry of Cardiopulmonary Resuscitation, I. (2008) Survival from in-hospital cardiac arrest during nights and weekends. JAMA, 299(7),(pp. 785-792)
Ensuring a single standard of care, equalizing for health care system disparities
Nurses in NICUs face inadequate staffing. They are more likely to miss required nursing care. Improving staffing and workloads may improve the quality of care for the infants born in high-black hospitals.
--Lake, E. T., Staiger, D., Edwards, E. M., Smith, J. G., & Rogowski, J. A. (2017). Nursing Care Disparities in Neonatal Intensive Care Units. Health Services Research. Retrieved August 14, 2018, from doi:10.1111/1475-6773.12762
The hospitals that disproportionately cared for Hispanics were more than three times as likely as others to be for profit and less likely to have medical or cardiac ICUs. Hospitals that care for high proportions of Hispanic patients had much lower nurse staffing levels. The investigators also found that hospitals caring for high proportions of Hispanic patients also had lower patient outcome performance in the areas of CHF, acute MI, and pneumonia.
--Jha, A. K.; Orav, E. J.; Zheng, J.; & Epstein, A. M. (2008) The Characteristics and Performance of Hospitals that Care for Elderly Hispanic Americans. Health Affairs (Millwood), 27(2), (pp. 528-537) Retrieved August 14, 2018, from doi:10.1377/hlthaff.27.2.528
Older black adults who undergo elective hip or knee replacement are more likely to experience a 30-day unplanned readmission than their white counterparts. For all older adults, being cared for by a nurse with a heavier workload is associated with greater odds of readmission, although the deleterious effects of less-favorable staffing is more pronounced for older black adults. Efforts to reduce unplanned readmissions after elective joint replacement should include heightened attention to the role of nursing care, particularly for older minority populations.
--Silber, J., et al. (2015) Examining Causes of Racial Disparities in General Surgical Mortality: Hospital Quality Versus Patient Risk. Medical Care, 53(7), (pp. 619-629) Retrieved August 14, 2018, from doi:10.1097mlr.0000000000000377
Better nurse staffing is associated with survival for black patients and diminishes racial disparities in survival after in-hospital cardiac arrests medical care.
--Brooks Carthon, Margo PhD, APRN, FAAN; Brom, Heather PhD, APRN; McHugh, Matthew PhD, JD, MPH, RN, FAAN; Sloane, Douglas M. PhD; Berg, Robert MD; Merchant, Raina MD, MHSP, FAHA; Girotra, Saket MD, SM; Aiken, Linda H. PhD, FAAN, FRCN; et al. Medical Care. 59(2):169-176, February 2021.
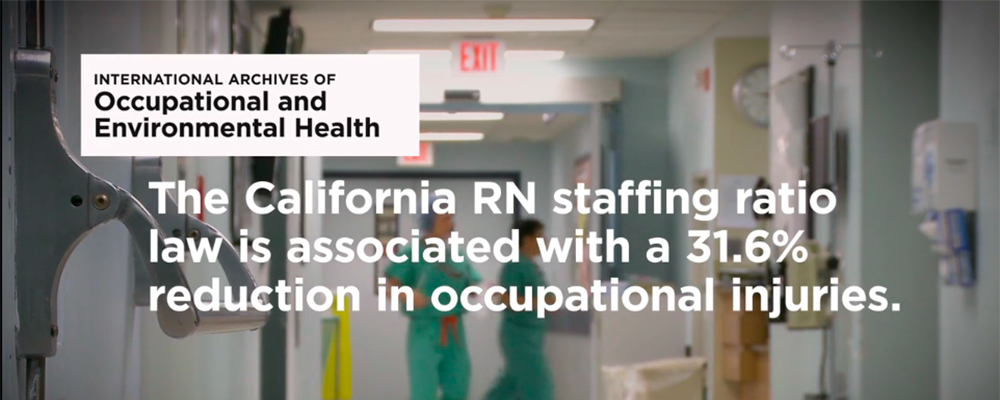
Making nurses healthier
A 2015 study, which examined occupational injury and illness rates before and after the California RN staffing ratios law was passed, showed what RNs already know — safer nurses means safer patients. Examining data from all 50 states, the study also found that the California RN staffing ratios law was associated with a 31.6 percent reduction in occupational injuries and illnesses among RNs working in hospitals in California.
--Leigh, J. P.; Markis, C. A.; Losif, A. M.; & Romano, P. S. (2015) California’s Nurse-to-Patient Ratios Law and Occupational Injury. International Archives of Occupational and Environmental Health, 88(4) (pp. 477-484)NICU infection rates. JAMA Pediatrics, 167(5), (pp. 444-450) Retrieved August 14, 2018 from doi:10.1001/jamapediatrics.2013.18
An increased patient load per nurse was associated with significantly higher likelihood for neck, shoulder, and back musculoskeletal disorders.
--Lipscomb, Trinkoff, Brady, & Geiger-Brown, 2004
Risk for workplace violence injuries was twice as high for lower-staffed hospitals as compared to higher-staffed hospitals.
--Lee, Gerberich, Waller, Anderson, & McGover
Accept no substitutes for nursing care!
What’s the link between nurse staffing and patient mortality? Simple: missed nursing care. Decades of studies have shown that more nurses equate to lives saved and fewer complications. After ratios were implemented, research demonstrated that ratios were working. Now, researchers have been focusing on the link between increasing RN staffing and improved outcomes. It’s no surprise to us that, once again, more studies have echoed what nurses have always said, “Care is being left undone.”
In fact, in 2018, results from an observational study exploring the relationship between nurse staffing, missed care, and mortality published in the International Journal of Nursing Studies validates this link. The authors report that “Research spanning decades has reported that lower registered nurse (RN) staffing is associated with higher levels of case-mix adjusted patient mortality. Lower RN staffing is also associated with a greater risk that necessary nursing care is missed due to lack of time.” The study found that “missed nursing care is a mediator in the relationship between nurse staffing and mortality.” The authors note that the study is “building on earlier previously published findings from an observational study of 422,730 patients who underwent common surgeries in 300 European hospitals, this paper provides evidence of an association between missed nursing care and postsurgical mortality.”
--Ball, Jane E., et al. Post-Operative Mortality, Missed Care and Nurse Staffing in Nine Countries: A Cross-Sectional Study. International Journal of Nursing Studies, Vol. 78, (pp. 10-15)
Minimum nurse-to-patient ratio policies are a feasible approach to improve nurse staffing and patient outcomes with good return on investment.
--Matthew D McHugh; Linda H Aiken; Douglas M Sloane; Carol Windsor; Clint Douglas; Patsy Yates; et al. Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: a prospective study in a panel of hospitals, May 11 2021
