Press Release
Nurses face worsening working conditions amid winter surge in Covid and other respiratory viruses, as CDC looks to weaken infection control guidance
Ninth National Nurses United Covid survey points to continued egregious lack of protections
As Covid and other respiratory viruses are surging once again, National Nurses United’s (NNU) latest nationwide survey of more than 2,600 registered nurses reveals continued failure by health care employers to protect staff and patients from Covid-19, other significant safety issues, and the ongoing deleterious effects of the pandemic on the emotional and physical health of nurses.
These already dangerous working conditions for nurses are likely to be worsened if the Centers for Disease Control and Prevention (CDC) fails to reject draft updates from its advisory committee on health care infection control (HICPAC). HICPAC’s draft, which was finalized by a unanimous vote in November 2023, proposes to weaken existing protections and ignores scientific evidence on aerosol transmission and respiratory protection.
This is the ninth national survey of nurses conducted by NNU since the start of the Covid pandemic. This survey finds that employers continue to fail to institute basic protective measures for Covid-19, including contact tracing, screening, and personal protective equipment (PPE). Results indicate that nurses continue to experience the impacts of long Covid, which can be debilitating and require nurses to take significant time off work to recover, contributing to the staffing crisis in health care.
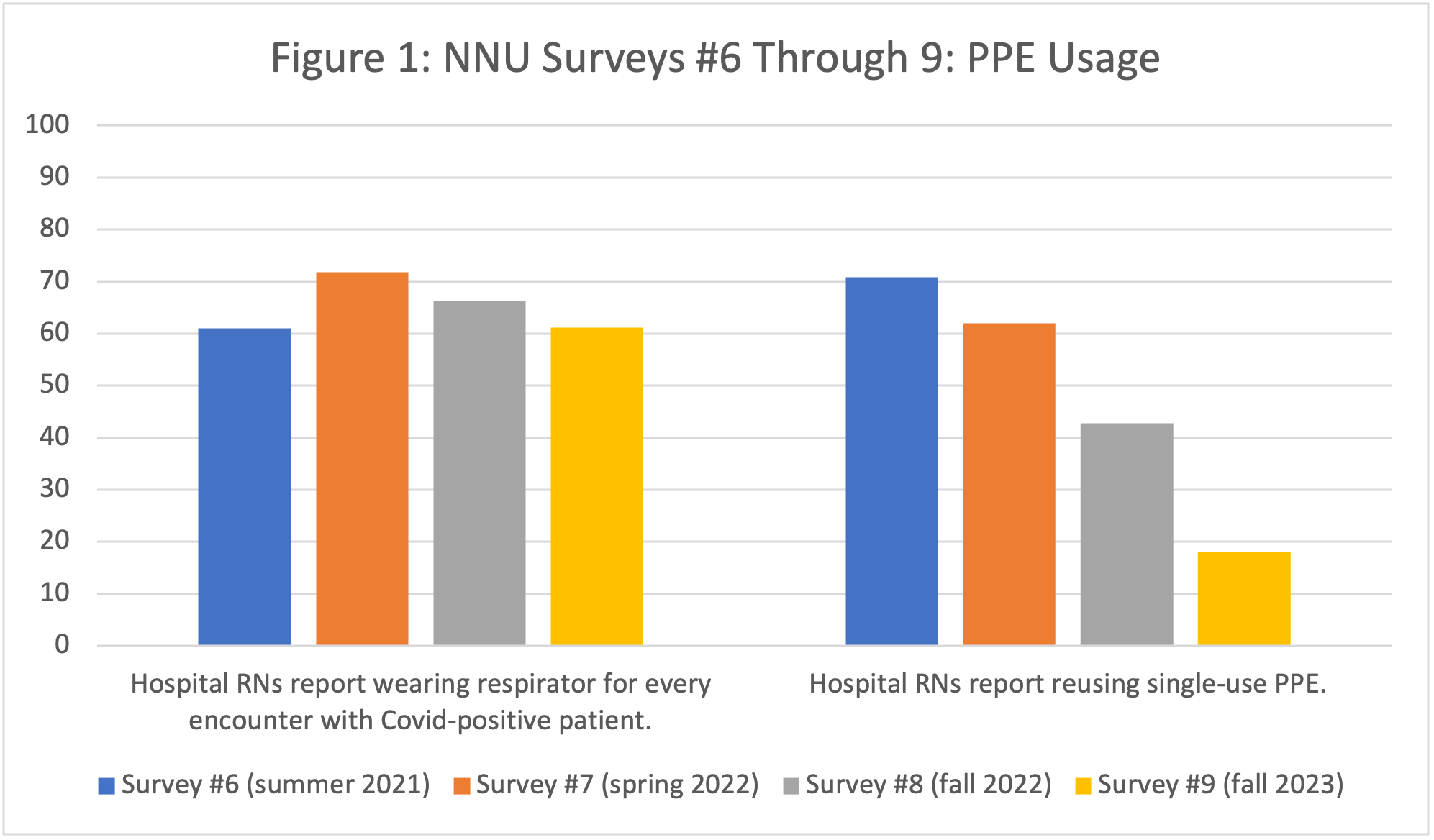
Specifically, NNU’s survey found only 61.2 percent of hospital nurses report wearing a respirator for every encounter with a Covid-positive patient, despite ample scientific evidence that a respirator is necessary PPE. This result underlines the issues with HICPAC’s draft guidance updates, which seek to limit the use of lifesaving respirators for health care workers caring for patients with pathogens that can be transmitted through the air—instead, relying on loose-fitting, unprotective surgical masks.
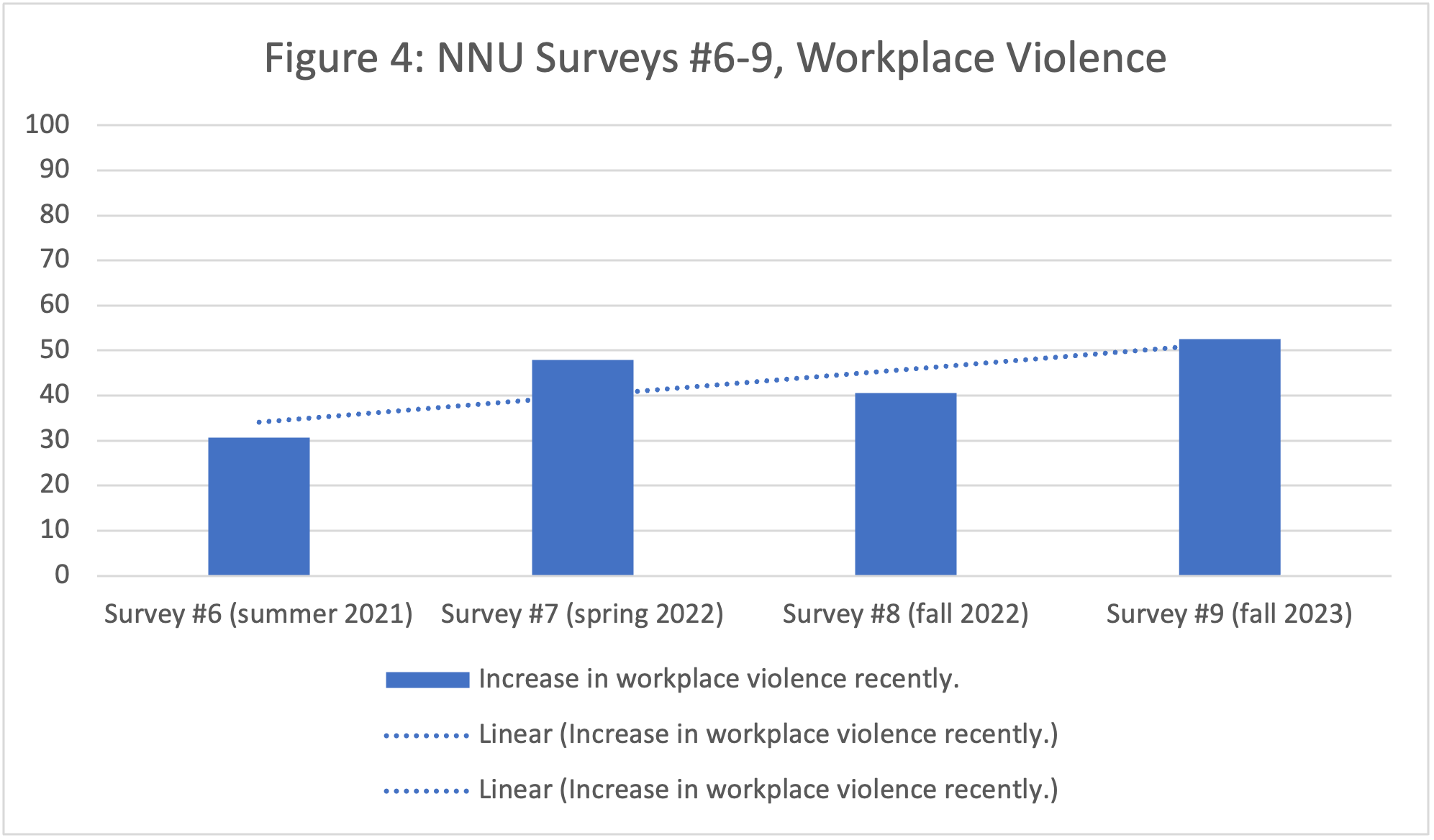
NNU’s survey finds that rates of workplace violence and unsafe staffing continue to worsen. 63.2 percent of hospital RNs report that staffing has gotten worse in their unit in the past month and 52.6 percent of hospital RNs report an increase in workplace violence recently.
Strikingly, nurses continue to report significant harm to their mental and physical health due to the pandemic, including trouble sleeping, anxiety and depression, and intention to leave their jobs or the profession entirely.
NNU’s ninth Covid survey underlines the damage caused by health care employer neglect of nurse health and safety. Stronger, not weaker, standards are necessary. The CDC must reject HICPAC’s draft. A permanent OSHA Covid standard must be issued.
Full Results of NNU’s Ninth Covid Survey:
Responses were gathered from 2,656 registered nurses, both NNU union nurses and nonunion nurses, in 50 states plus Washington, D.C. and Puerto Rico. The survey covers the period from August 18, 2023 through November 30, 2023.
Testing and Screening for Covid-19
- Only 31.2 percent of RNs report that all nurses are informed of exposures in a timely fashion. 29.0 percent of RNs report that nurses are informed of exposures but not in a timely fashion. Nearly one in four (24.9 percent) RNs report that nurses are not informed of exposures at all. Timely notification of an exposure to Covid is essential for preventing onward transmission.
- Nearly half (44.6 percent) of RNs report that their employer does not screen patients or visitors for Covid-19, even though research indicates that screening is an important measure to prevent Covid-19 transmission in health care facilities.
- The proportion of nurses reporting timely exposure notification and patient/visitor screening have remained consistently low in NNU’s surveys conducted in 2021, 2022, and 2023, indicating that health care employers continue to neglect these important prevention measures.
Personal Protective Equipment
- Only 72.4 percent of hospital RNs report having access to a sufficient supply of N95 or other kinds of respirators on their unit. Ready access to PPE, including N95 respirators, is a necessary element in keeping RNs and other health care workers safe from Covid exposure.
- Only 61.2 percent of hospital RNs report wearing a respirator for every encounter with a Covid-positive patient. It is scientifically clear that Covid-19 is transmitted through respiratory aerosols created when people infected with the virus breath, speak, cough, sneeze, etc. and that respiratory protection is a necessary element in keeping RNs and other health care workers safe from Covid-19. The proportion of nurses reporting respirator use for Covid-positive patients has declined from a peak of 71 percent in the spring of 2022 (Figure 1), indicating that health care employers continue to fail to implement this essential, lifesaving measure to protect staff and patients.
- Reusing single-use PPE is an unsafe practice that should never occur. Nearly one in five (18.0 percent) hospital RNs report still having to reuse single-use PPE such as N95 respirators, isolation gowns, and gloves. While this is a significant decline from surveys conducted in 2021 and 2022 (Figure 1) https://www.nationalnursesunited.org/nnu-covid-survey-8, which found that 42.8 to more than 70 percent of hospital RNs reported reusing single-use PPE, it is still concerningly high.
Long Covid
- 69.5 percent of RNs report having been diagnosed with Covid-19. Of those who had Covid, 56.4 percent had Covid once, 29.8 percent twice, 10.5 percent three times, 2.0 percent four times, and 1.4 percent five or more times. This is likely an undercount due to lack of testing and asymptomatic cases.
- After recovery from Covid-19, RNs experienced ongoing symptoms, including tiredness or fatigue, memory or concentration difficulties, joint or muscle pain, headaches or migraines, difficulty breathing or shortness of breath, symptoms that get worse after physical or mental activities, heart palpitations, and chest pain. These symptoms have lasted: 0-3 months for 30.8 percent of RNs, 4-6 months for 13.7 percent of RNs, 7-9 months for 5.8 percent of RNs, 10-12 months for 7.4 percent of RNs, and more than 12 months for 28.1 percent of RNs.
- A majority of RNs (58.4 percent) who had Covid at least once required time off work to recover from post-Covid symptoms.
- For 53.1 percent of RNs who had Covid, their long Covid symptoms have affected their ability to work. And for 65.1 percent of RNs, their long Covid symptoms have impacted their daily activities outside of work.
Staffing
- A majority of nurses continue to report unsafe staffing in their facilities—63.2 percent of hospital RNs report that staffing has gotten slightly or much worse in the past month. This result has remained consistent in surveys conducted in 2021, 2022, and 2023 (Figure 2), indicating that health care employers continue to fail to safely staff units, which jeopardizes nurse and patient safety.
- 30.6 percent of hospital RNs report an increase in the use of travelers in the past month, which is a decrease from surveys conducted in 2021 and 2022 (Figure 2).
- 14.5 percent of hospital RNs report that their facility has introduced new models of nursing, e.g., team nursing, or other “crisis staffing standards” in the past month. This is a slight increase from surveys conducted in 2021 and 2022.
- Nearly half (47.3 percent) of hospital RNs report that their facility is using excessive overtime to staff units. This result is essentially unchanged from surveys conducted in 2021 and 2022, indicating that health care employers continue to fail to safely staff units.
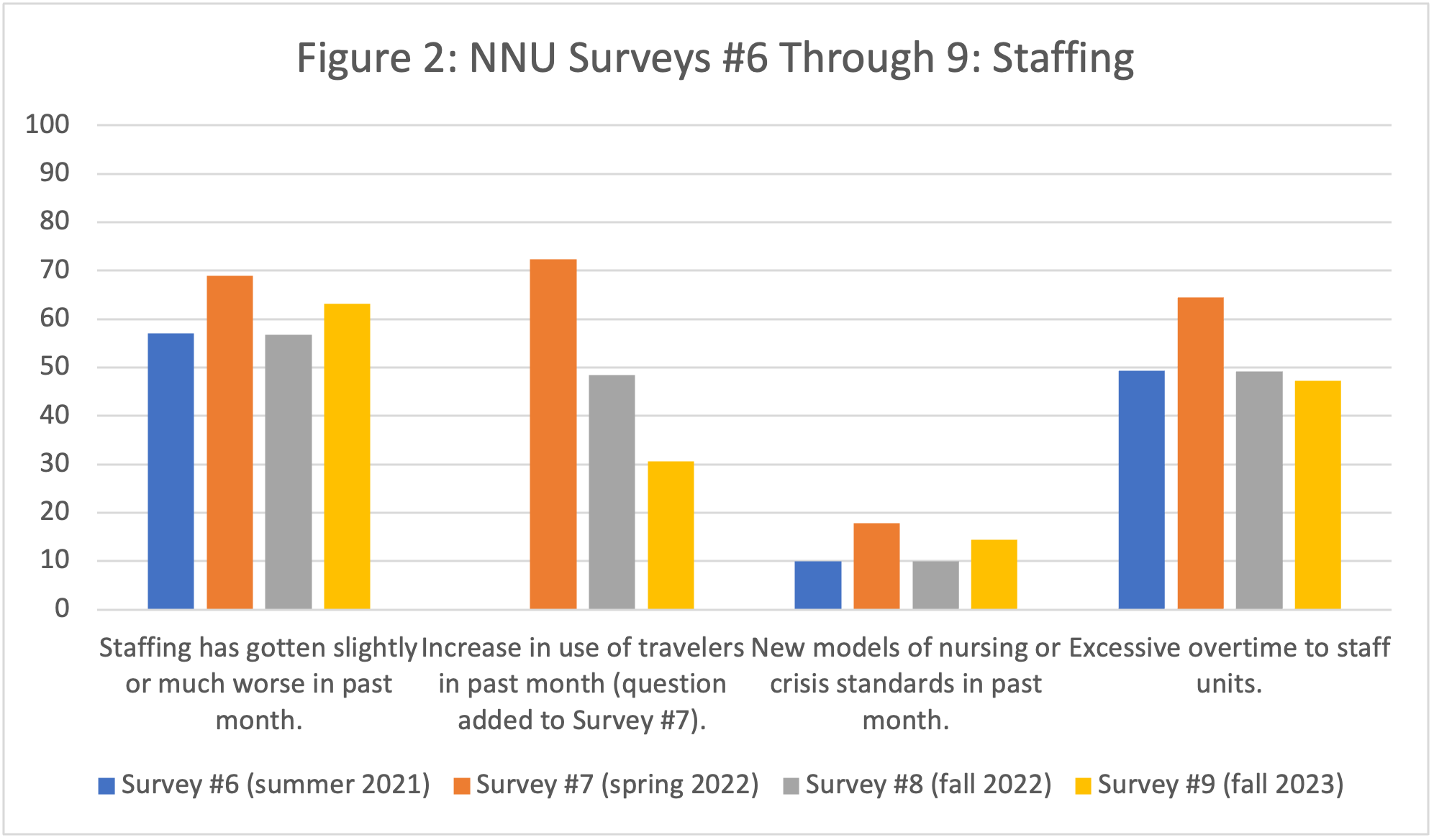
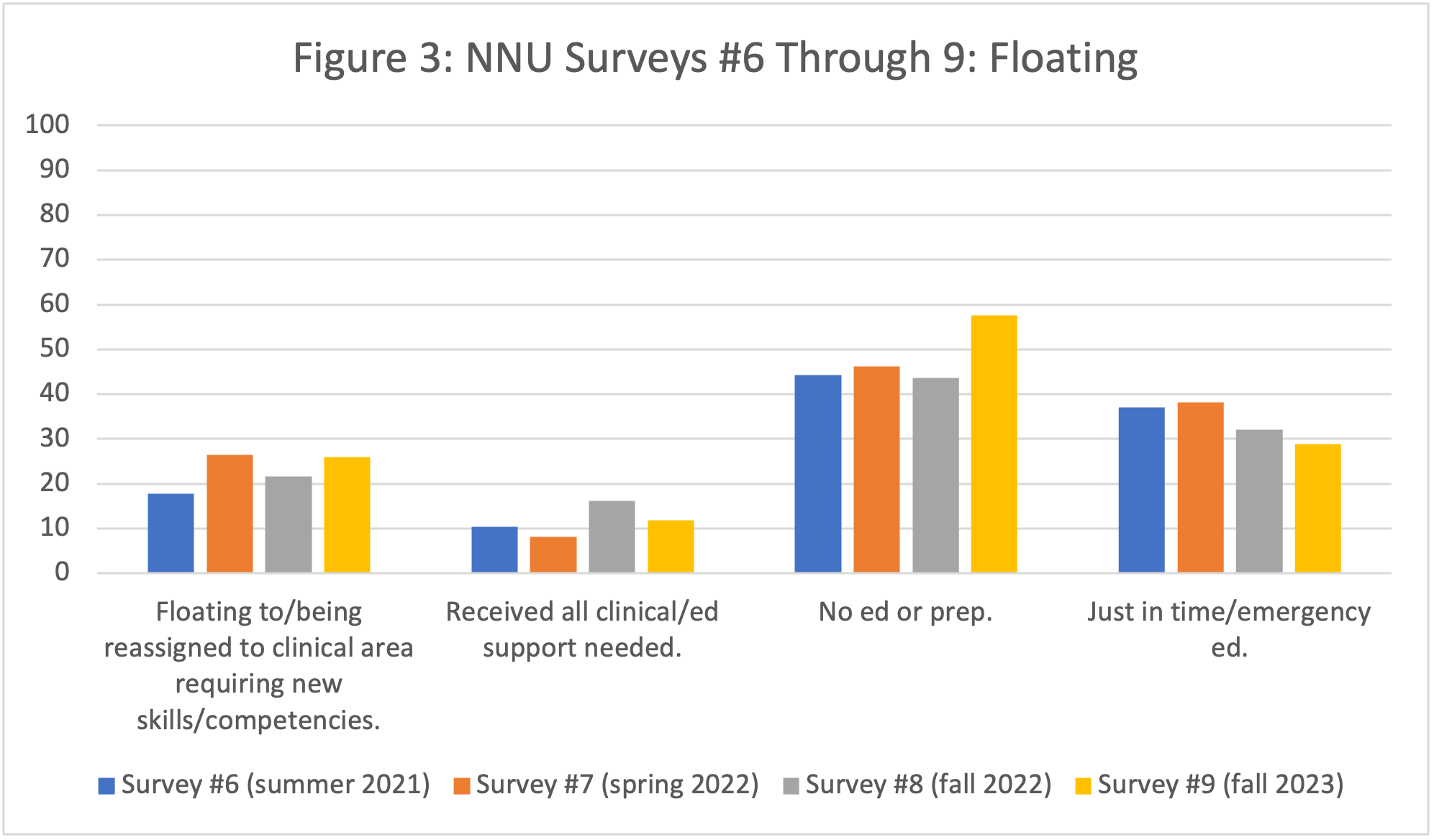
- The following results are nearly unchanged from NNU’s 2021 and 2022 surveys (Figure 3), indicating that hospitals continue to rely on unsafe measures to staff units.
- 26.0 percent of hospital RNs report floating to/being reassigned to a clinical care area where they were expected to care for patients that required new skills or competencies.
- Only 11.9 percent of hospital RNs reported receiving all the clinical and educational support that they needed to practice safely and competently. Most nurses received either no education or preparation (57.6 percent) or “just in time” or “emergency” competency education (28.9 percent).
Impacts of the Pandemic
- 52.6 percent of hospital RNs report a small or significant increase in workplace violence incidents recently. The proportion of nurses who have reported a recent increase in workplace violence incidents has risen significantly since 2021 (Figure 4).
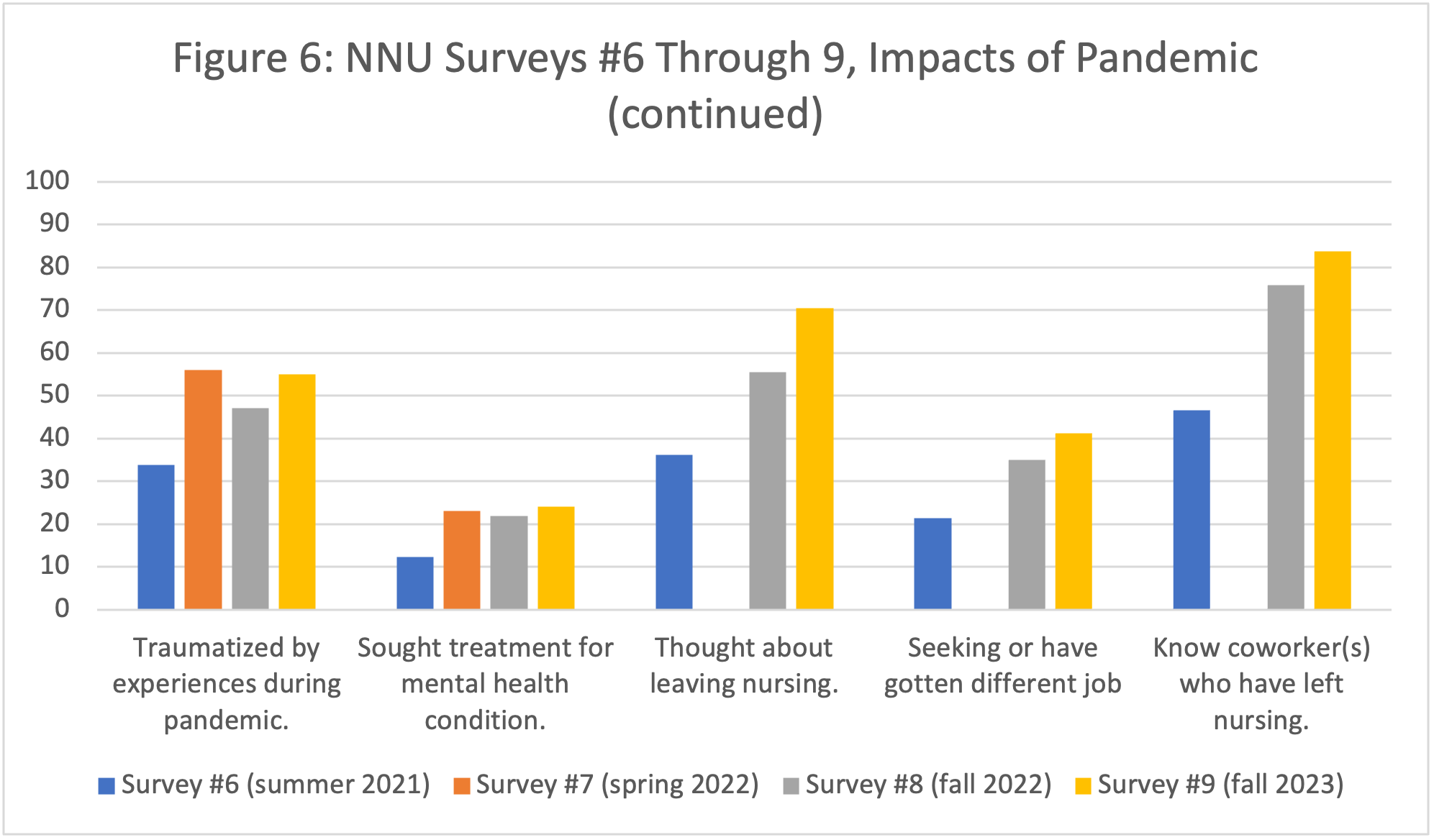
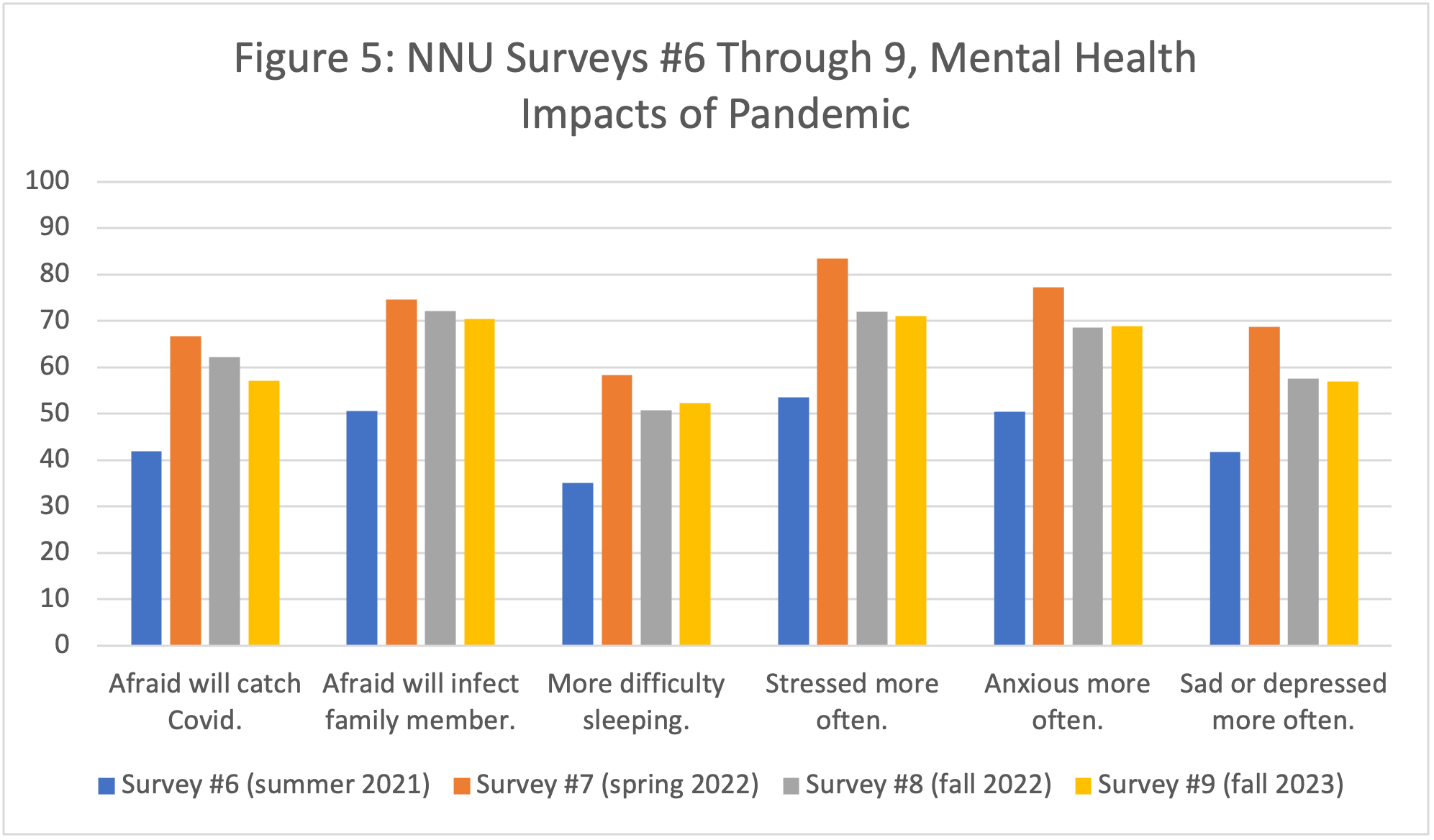
- Nurses continue to experience significant impacts of the Covid-19 pandemic on their mental and physical health. While many of these results have declined slightly since the spring of 2022 (Figures 5 and 6), all remain at high levels, indicating ongoing harm to nurses’ health.
- 57.1 percent of RNs report they are afraid they will catch Covid-19.
- 70.4 percent of RNs report they are afraid they will infect a family member with Covid-19.
- 52.3 percent of RNs report having more difficulty sleeping than they did before the pandemic.
- 71.0 percent of RNs report feeling stressed more often than they did before the pandemic.
- 68.9 percent of RNs report feeling anxious more often than they did before the pandemic.
- 56.9 percent of RNs report feeling sad or depressed more often than they did before the pandemic.
- 55.0 percent of RNs report feeling traumatized by their experiences caring for patients during the pandemic.
- 24.1 percent of RNs report having sought treatment for a mental health condition related to caring for patients during the pandemic.
- Many nurses cite impacts of the pandemic—and specifically their employers’ ongoing failures to safely staff their units and provide strong workplace protections—as reasons they are considering or have left the bedside. NNU’s ninth Covid survey finds significant and substantial increases in the proportion of nurses who report considering or actively seeking to leave their current position (Figure 6).
- 35.3 percent of RNs report they have reduced the number of hours they are working as a nurse.
- 70.4 percent of RNs report they have thought about leaving nursing.
- 41.2 percent of RNs report they are seeking or have gotten a different job.
- 46.4 percent of RNs report that they are seeking or have gotten a different type of nursing job.
- 83.8 percent of RNs know coworker(s) who have left nursing.